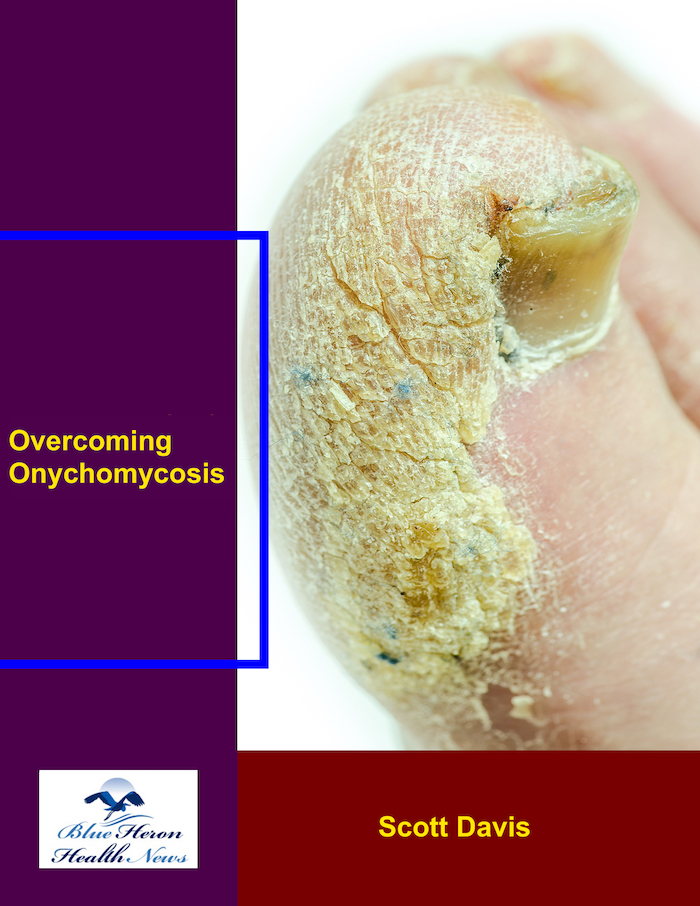
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is the prognosis for proximal subungual onychomycosis?
The prognosis of proximal subungual onychomycosis (PSO) typically depends on the severity of the infection, the etiologic fungi, the timeliness of treatment, and the overall health of the patient. PSO is a fungal infection of the nail matrix (tissue beneath the nail base) and usually begins at the proximal (base) of the nail, usually with white or yellow coloration and extending toward the distal edge of the nail.
Prognosis Factors for Proximal Subungual Onychomycosis:
1. Early Diagnosis and Treatment:
Early intervention is necessary in preventing the infection from spreading and causing permanent nail damage. The result is considerably improved if the treatment is initiated early.
Treatment with oral antifungals (e.g., terbinafine or itraconazole) is generally more successful for PSO, as it targets the fungal infection from the inside of the nail bed and matrix.
If left untreated or if the treatment is delayed, the infection will be more difficult to treat and can lead to permanent nail damage or nail loss.
2. Fungus Type:
PSO is usually caused by dermatophytes (fungi like Trichophyton rubrum), but can also be caused by yeasts or non-dermatophyte molds. The type of fungus that causes the infection can affect the success of the treatment.
Dermatophyte infections are typically easier to cure and are more likely to have a better prognosis than yeasts or molds, for which the infection may require a longer or alternative treatment regimen.
3. Severity of Infection:
PSO that is mild in severity with limited involvement of the nail also carries an excellent prognosis and can be treated with topical or oral antifungals.
Severe or chronic infections that have caused massive damage to the nail matrix can cause permanent deformities of the nail, such as thickening, pigmentation, or total permanent loss of the nail.
4. Immune Status:
Those patients with compromised immune status (e.g., diabetes, HIV/AIDS, or chemotherapy) will be harder to treat and can be susceptible to recurrent infection or complications.
In patients with unimpaired immune systems, the infection is usually more amenable to treatment, and the prognosis is improved.
5. Adherence to Treatment:
Adherence to the treatment schedule is vital for successful outcome. Treatment for PSO is typically long-term (often months) to clear the infection entirely. Skipping doses or discontinuing treatment prematurely can lead to relapse or partial clearing of the infection.
6. Damage to the Nail:
In more severe cases of PSO, especially if left untreated for a long period of time, the nail matrix (that area of the nail from which it emerges) may suffer permanent damage, leading to permanent nail deformity or loss of a nail.
However, if treated and diagnosed early on, the nail usually heals and infection is cured with minimal long-term damage.
7. Recurrence
Despite effective treatment, recurrence of PSO is not unusual, especially if the underlying fungal environment (e.g., wet or unclean) is not removed.
Prevention can be ensured by the individual through measures such as drying of the nails, not sharing personal items, and frequent use of antifungal medication, in order to avoid reinfection.
General Prognosis
Good Prognosis: If diagnosed early and treated with the appropriate antifungal medications (oral or topical), PSO generally has a good prognosis, and most patients achieve complete resolution with restoration of the nail.
Poor Prognosis: In case the infection has caused significant damage to the nail matrix or if the infection is allowed to run for prolonged periods without any treatment, the prognosis may be poor, with possibilities of permanent alteration of the nail or loss of the nail.
The outcome of proximal subungual onychomycosis is generally good with early treatment and effective antifungal therapy. If the infection is treated early, the infection can be eradicated without causing permanent damage. However, if the infection is advanced or untreated, it may lead to severe nail damage or permanent modification. Prevention and adherence, like in all fungal infections, are necessary to ensure a good result.
Endonyx onychomycosis is one type of nail fungal infection that primarily affects the nail plate, tending to create structural deformities in the nail. It is where the fungus penetrates into the inner part of the nail plate rather than on the exterior or beneath the nail. Such a type of onychomycosis has the capability of inducing severe deformity to the nail and may be difficult to diagnose since its initial characteristics are not observable. This is how it affects the nail’s structure:
1. Fungal Infection of the Nail Plate:
In endonyx onychomycosis, the fungus infects the nail plate, rather than the nail bed or nail matrix (the area where the nail is formed). This can be more difficult to diagnose in its early stages because the infection is hidden inside the nail.
The fungal organisms, such as dermatophytes, typically infect the keratin layers of the nail, disturbing its internal structure.
2. Thickening and Brittleness:
The infection tends to thicken the nail plate and render it hard and brittle.
The nail can become opaque, yellowish, or whitish in appearance as the infection progresses and the fungal invasion breaks through inside the nail.
The nail could also crumble or break more easily, particularly at the edges, due to its compromised composition.
3. Changes in Nail Texture:
Endonyx onychomycosis results in a change in the texture of the nail plate. The nail plate will become irregular, rougher, or pitted as the fungal infection damages the inner keratin layers of the nail.
These alterations will dull and distort the shape of the nail.
4. Nail Plate Separation:
As the infection progresses, the nail plate may begin to loosen from the nail bed, a condition known as onycholysis. This may lead to partial loosening of the nail from the tissue underneath.
However, in endonyx onychomycosis, loosening is normally less noticeable at the edges compared to other types of onychomycosis, since the infection only occurs within the inner nail structure.
5. Onycholysis of a fine nature
In contrast to all other forms of onychomycosis except for endonyx onychomycosis, endonyx onychomycosis is not usually marked by any apparent coloration of the nail or complete detachment from the nail bed at the nail’s edge. Rather, changes within the internal nail structure may create an indistinct or not easily visible elevation of the nail from the nail bed.
6. Possible Nail Abnormalities
Deformation of the nail may occur over time due to the infection causing interruption to the normal development and growth of the nail.
Deformation, misshapening, or the formation of abnormal curvatures of the nail may occur as the fungus causes weakening and destruction of nail structure.
7. Long-Term and Chronic Infections:
The fungal infection, if left untreated, continues to cause progressive damage to the nail, leading to more severe nail deformities.
In severe cases, the nail can actually break down completely and the individual loses the nail.
8. Potential Complications:
Even though endonyx onychomycosis affects the nail plate, it can also potentially result in secondary infection if the fungus goes on to infect other parts of the nail or surrounding skin.
Destruction of the nail structure also exposes the individual to trauma or other fungal infections.
Conclusion:
Endonyx onychomycosis involves the internal nail plate matrix, leading to thickening, brittleness, and textural modifications. The fungus infects the nail’s keratin layers, causing mild deformities and internal damage rather than always leading to obvious separation or discoloration at the margins. Early diagnosis and treatment are necessary to prevent permanent nail structure damage and reduce the risk of severe infection.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!