Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What are the symptoms of endonyx onychomycosis?
Endonyx onychomycosis is one of the types of dermatophyte infection of the nail plate (the hard outer part of the nail). Unlike other forms of onychomycosis, endonyx infects the nail from within, and the alterations may be less noticeable at the beginning. Symptoms range from mild to severe but typically appear as follows:
1. White or Yellowish Discoloration:
The nail plate may begin to appear white or yellowish, especially in the center of the nail. Discoloration is caused by fungal growth under the nail plate.
The nail may not show the typical superficial white spots of other forms of onychomycosis but rather may show internal discoloration that progresses along the nail as the infection persists.
2. Thickening of the Nail Plate:
One of the typical signs of endonyx onychomycosis is thickening of the infected nail. The nail is elevated and seems to be bulging.
The excess thickness makes the nail more difficult to cut and, depending on the extent of the infection, may be painful or cause pressure.
3. Loss of Shine:
The infected nail loses its natural shine and becomes opaque or dull. The changed appearance gives the nail an unhealthy appearance.
4. Nail Detachment from the Nail Bed (Onycholysis):
As the fungus continues to grow, the nail plate may begin to detach from the nail bed. This is known as onycholysis.
Detachment can cause a space between the nail and the tissue around it, with a high chance of secondary infection and susceptibility to injury to the nail.
5. Nail Fragility:
The involved nail may become brittle, crumbly, or cracked. It becomes susceptible to chipping or breaking as the infection becomes stronger.
The nail will be weak and delicate to the touch. Even slight damage can lead to the nail splitting or cracking.
6. Curving of the Nail Shape
In extreme cases, the nail may be deformed in shape. The normal curvature of the nail may become abnormal since the fungal infection compromises the nail structure.
The nail may grow irregularly or unevenly, which makes it appear deformed.
7. Discomfort or Pain (Uncommon):
Endonyx onychomycosis is generally less painful than some other types of fungal nail infections. With secondary bacterial infection or onycholysis associated, in more severe cases, the patient will have mild pain or tenderness, particularly if pressure is being exerted (e.g., when putting on shoes).
8. Slow Progression:
The infection becomes more advanced slowly, and the symptoms manifest progressively over time. This allows ignoring it in the early phases, and many don’t see a doctor until the infection has caused noticeable changes in the nail.
9. Involvement of Multiple Nails:
Endonyx onychomycosis typically affects one or multiple nails, most commonly the toenails, but fingernails can also be involved. It is less probable to affect all nails at the same time.
Diagnosis:
Endonyx onychomycosis is diagnosed typically by clinical examination, but microscopic examination or culture of the nail clip may be needed to confirm the etiologic fungal pathogen of the disease.
Dermatophytes are most often the causative organisms of endonyx onychomycosis, although at times the non-dermatophyte fungi are involved.
Treatment:
Endonyx onychomycosis, especially the mild variety, may be treated successfully with topical antifungal medication (amorolfine, ciclopirox, or terbinafine).
Oral antifungal medications (like terbinafine or itraconazole) may be prescribed for more severe or chronic infections.
To avoid infection, keep your nails trimmed and clean, wear well-ventilated shoes, and don’t over-moisturize.
You should have a medical professional or dermatologist consult if you think you have endonyx onychomycosis, so you can receive a proper diagnosis and treatment plan.
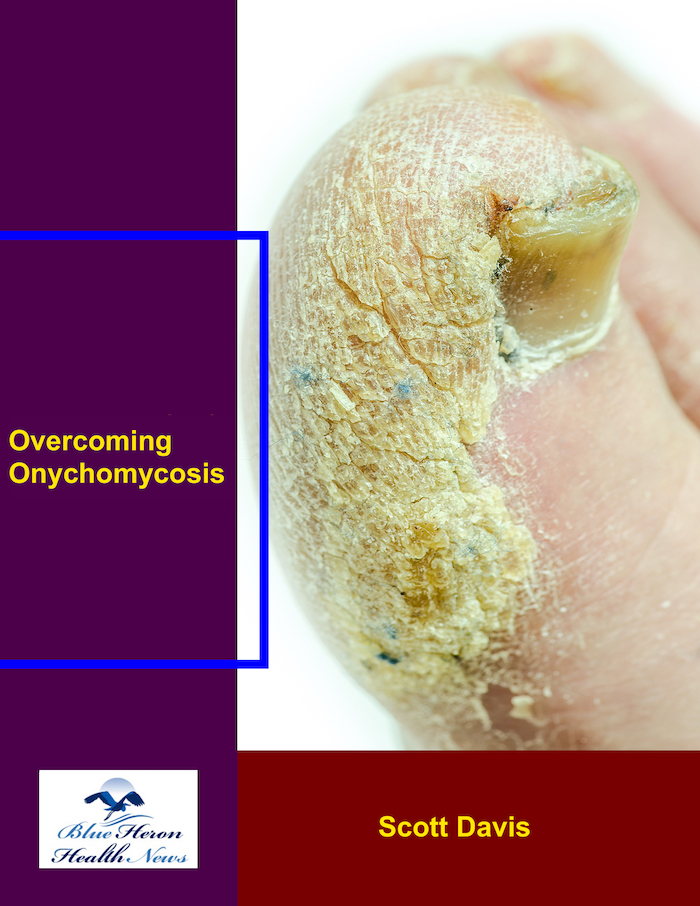
Total Dystrophic Onychomycosis (TDO) is the most severe form of onychomycosis, or fungal nail infection. It is the worst form of a not-treated or poorly-treated fungal nail infection. TDO is characterized by extensive nail destruction and deformation. This is how it happens:
1. Initial Infection:
Development of TDO is typically preceded by an infection of the nail bed or nail plate by a fungal infection, which is typically initial distal subungual onychomycosis (DSO) or proximal subungual onychomycosis (PSO). The infection is typically caused by dermatophytes (e.g., Trichophyton rubrum) or, less commonly, yeast or non-dermatophyte molds.
The infection typically begins with subtle symptoms, such as discoloration (yellow, white, or brown), thickening, and crumbling at the edge of the nail.
2. Progression of Infection:
If not treated or inadequately treated, the infection progresses with the fungus extending deeper into the nail plate and nail bed. It may infect deeper structures, including the nail matrix (the area where the nail is formed), causing permanent damage.
The nail may thicken, become discolored, and brittle, leading to increased separation of the nail from the nail bed (onycholysis).
As the fungal infection progresses and causes more harm to the nail, it can lead to deformity, loss of nail shape, and even complete destruction of the nail plate. The nail becomes opaque, crumbly, and brittle, which is characteristic of TDO.
3. Total Nail Destruction:
During the late stages, the fungal infection can completely devastate the entire nail. The nail may even become completely separated from the nail bed, laying bare the underlying tissue. This stage is referred to as total dystrophic onychomycosis.
The nail may become thickened, deformed, and smaller, with white or yellowish pigmentation.
Pain, swelling, and redness in the nail fold and the surrounding tissue may be present.
4. Contributing Factors:
Immune System Deficiency: Individuals with weakened immune systems, such as individuals with diabetes, HIV, or individuals on immunosuppressive treatment, are more likely to get TDO because their bodies cannot fight the fungal infection as effectively.
Chronic Conditions: Circulatory insufficiency, diabetes, and peripheral neuropathy increase individuals’ susceptibility to infection and can delay detection and treatment of the infection.
Inadequate or Mistaken Treatment: If the infection is not properly treated with oral antifungals or topical creams, the fungus continues to develop and create deep damage to the nail that finally leads to TDO.
5. Symptoms and Appearance of TDO:
Severe Thickening: The nail gets very thick, typically with an irregular surface.
Discoloration: The nail becomes discolored, typically yellow, white, or even black.
Deformation: The form of the nail is altered, with fraying borders, and may lose its normal appearance.
Separation: The nail splits from the nail bed (onycholysis), becoming susceptible to bacterial infection.
Pain and Discomfort: Pain could be experienced in certain cases, particularly when the nail is broken or infected tissue beneath it.
6. Diagnosis:
Diagnosis of TDO is traditionally made on the basis of clinical observation of the nail, but firm diagnosis is always made using nail scraping or biopsy to identify the causative fungus by microscopy or culture.
Confirmation of infection by fungus can be done by KOH preparation or culture of the nails.
7. Treatment:
Oral Antifungal Drugs: Oral antifungal medications such as terbinafine, itraconazole, or fluconazole are commonly employed in the treatment of TDO.
Nail Debridement: In some cases, debridement with surgery or nail avulsion may be required to aid in the process of healing and alleviate the symptoms.
Long-Term Therapy: Because of the severity of TDO, treatment is typically taking antifungal medication for a few months, and in some cases, the infection may recur if not completely eradicated.
8. Prevention and Management:
Early Detection: Early detection and treatment are necessary to prevent the progression of onychomycosis to TDO. If the infection is caught early, topical treatments can be effective, but for more severe cases, oral antifungal treatment is required.
Good Foot Hygiene: Keeping nails clean, trimmed, and dry decreases the risk of fungal infections.
Avoiding Nail Trauma: Injury or trauma to nails can result in increased risk for fungal infection, hence nails must be kept from injury.
Management of Underlying Conditions: Proper management of underlying conditions like diabetes or immune disorders may reduce the risk for infection.
Conclusion:
Total Dystrophic Onychomycosis (TDO) occurs as a severe sequel of untreated or under-treated onychomycosis, producing severe damage and destruction of the nails. The disease usually starts as distal or proximal subungual onychomycosis and, with time, extends to the nail plate, leading to deformation, thickening, and even loss of the nail. Early diagnosis, appropriate antifungal treatment, and adequate podiatric care have an important role in preventing this severe sequel of onychomycosis.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!