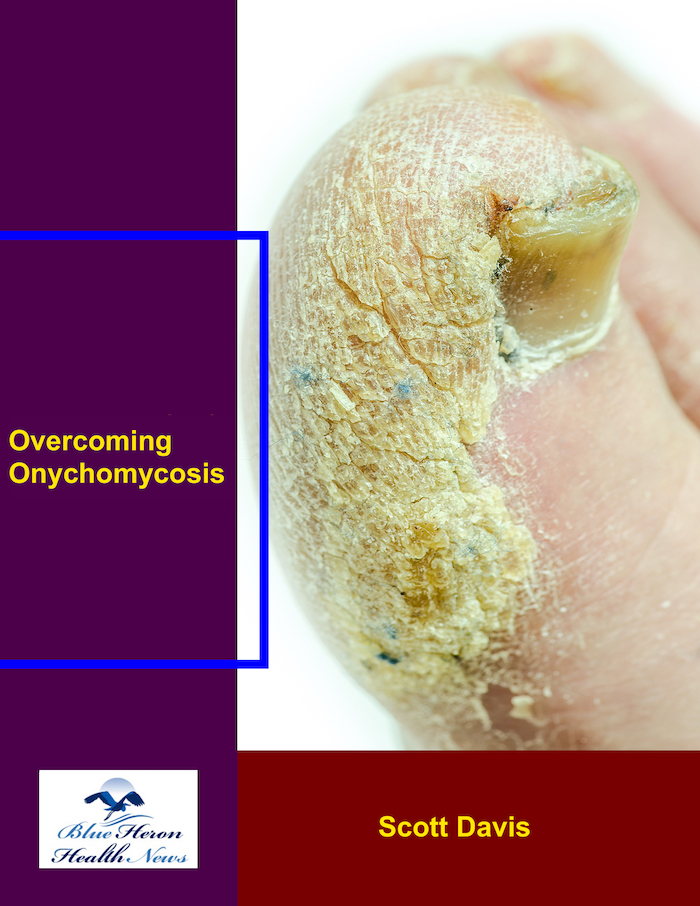
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
How does Candida species cause onychomycosis?
Candida species are a type of yeast that can cause onychomycosis, although they are less common than dermatophytes in causing nail infections. Candida-related onychomycosis often involves both nail and nail bed and may affect fingernails more frequently than toenails. Here’s how Candida causes onychomycosis:
1. Types of Candida Involved
- Candida albicans is the most common species responsible for nail infections, but other species such as Candida tropicalis, Candida glabrata, and Candida parapsilosis can also cause infections.
2. Pathogenesis of Candida Onychomycosis
- Candida species are opportunistic pathogens, meaning they tend to cause infections when the skin or immune system is compromised. For onychomycosis, Candida usually infects the nail through breaks or damage in the skin around the nail, such as from nail biting, trauma, or manicures.
- Moisture and warmth create an environment where Candida can thrive, making areas such as the nail folds, cuticles, and proximal nail beds more vulnerable.
- Candida can invade the nail plate and the nail bed, leading to thickening, discoloration, and other signs of infection. Unlike dermatophyte infections, which primarily affect the nail plate, Candida infections often involve the nail bed and surrounding tissues, causing inflammation and swelling.
3. Risk Factors for Candida Onychomycosis
- Immune suppression: Individuals with weakened immune systems, such as those with HIV, chemotherapy treatments, or organ transplants, are more likely to develop Candida-related onychomycosis.
- Diabetes: People with diabetes are at increased risk due to poor circulation and a weakened immune response, which makes it harder to fight off fungal infections, including Candida.
- Moisture exposure: Regular exposure to water or damp environments (e.g., dishwashers, swimming pools, or people who wash their hands frequently) can promote Candida growth around the nails.
- Nail trauma: Nail trauma, including frequent nail biting, manicures, or pedicures, increases the likelihood of infection by introducing Candida into the nail bed or cuticle.
- Poor nail hygiene: Failing to keep nails clean and dry or using artificial nails may increase the risk of developing Candida infections.
- Other dermatologic conditions: Psoriasis, eczema, or fungal infections like athlete’s foot can compromise the nail bed and make it easier for Candida to invade.
4. Clinical Features of Candida Onychomycosis
Candida infections of the nails can present with a variety of signs and symptoms:
- Proximal nail involvement: Unlike dermatophyte infections, Candida often affects the cuticle or nail folds first, causing redness, swelling, and pain.
- Thickened nails: As the infection progresses, the nail plate may become thickened, discolored (yellow or white), and brittle.
- Separation of the nail from the nail bed: In some cases, the infected nail may become loose and detach from the nail bed (onycholysis).
- Nail discoloration: Nails may appear white, yellow, or greenish due to Candida growth.
- Increased fragility: The nail may become fragile or crumbly, and it may break or chip easily.
- Paronychia (infection of the surrounding tissue): Candida infections often lead to paronychia, causing inflammation, swelling, and pain around the nail.
5. Diagnosis
- Microscopic examination: Nail scrapings or clippings can be examined under a microscope to identify Candida species, although this may not always be definitive.
- Culture: A fungal culture is the gold standard for diagnosing Candida onychomycosis. The sample taken from the affected nail can be cultured to identify the specific species of Candida causing the infection.
- PCR tests: Polymerase chain reaction (PCR) testing may be used for more accurate detection of Candida species, especially in difficult-to-diagnose cases.
6. Treatment of Candida Onychomycosis
Treatment for Candida-related onychomycosis typically includes topical and/or oral antifungal medications:
- Topical antifungals: Antifungal creams or lacquers containing clotrimazole, miconazole, ciclopirox, or amorolfine can be effective, particularly in mild cases.
- Oral antifungals: For more severe infections, oral antifungal medications like fluconazole, itraconazole, or terbinafine may be prescribed to penetrate the nail and treat the infection.
- Nail avulsion: In cases where the infection is severe or unresponsive to medication, nail removal may be considered to allow for better penetration of antifungal treatments and to remove the infected nail.
- Topical corticosteroids: If there is significant inflammation or swelling around the nail, a topical corticosteroid may be used to reduce inflammation.
7. Prognosis
- Candida onychomycosis can be chronic and difficult to treat. Success depends on factors such as the severity of the infection, the underlying health condition of the patient, and the timeliness of treatment.
- If treated early and effectively, Candida onychomycosis generally responds well to antifungal therapy, and the nail can regrow healthy.
- However, if left untreated, the infection can cause permanent nail damage or loss.
8. Prevention
Preventing Candida onychomycosis involves measures to reduce the risk of infection:
- Maintain good nail hygiene by keeping nails clean and dry.
- Avoid trauma to the nails and nail beds.
- Wear protective gloves in wet environments or when performing tasks that expose the hands to moisture.
- Treat underlying conditions like diabetes and immune suppression to reduce susceptibility.
- Avoid sharing personal items such as nail clippers or towels to reduce the risk of fungal transmission.
Conclusion:
Candida species cause onychomycosis by infecting the nail plate and surrounding tissues, particularly in individuals with compromised immune systems, moisture exposure, or nail trauma. The infection often presents with nail thickening, discoloration, and swelling of the cuticle or nail folds. Diagnosis involves microscopic examination and fungal cultures, and treatment typically includes topical or oral antifungal medications. Early treatment is important to prevent permanent nail damage, and prevention focuses on maintaining proper nail hygiene and avoiding trauma.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!