Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is the difference between onychomycosis and nail psoriasis?
Onychomycosis and nail psoriasis are two different conditions that affect the nails, but they have distinct causes, symptoms, and treatment approaches. Here’s a detailed comparison of the differences between the two:
1. Cause
- Onychomycosis (Fungal Nail Infection):
- Caused by Fungi: Onychomycosis is a fungal infection of the nails, typically caused by dermatophytes, but it can also be caused by yeasts (such as Candida) or non-dermatophyte molds. The infection often develops after exposure to fungi in moist environments (e.g., public pools, gyms) or from existing fungal skin infections like athlete’s foot.
- Infectious: Onychomycosis is contagious and can spread through direct contact with an infected person or contaminated surfaces.
- Nail Psoriasis:
- Caused by Psoriasis: Nail psoriasis is a manifestation of psoriasis, an autoimmune skin condition that causes rapid skin cell turnover and inflammation. In nail psoriasis, the immune system attacks healthy skin cells around and under the nails, leading to nail abnormalities.
- Non-Infectious: Unlike onychomycosis, nail psoriasis is not contagious. It results from a genetic predisposition and immune system dysfunction.
2. Appearance and Symptoms
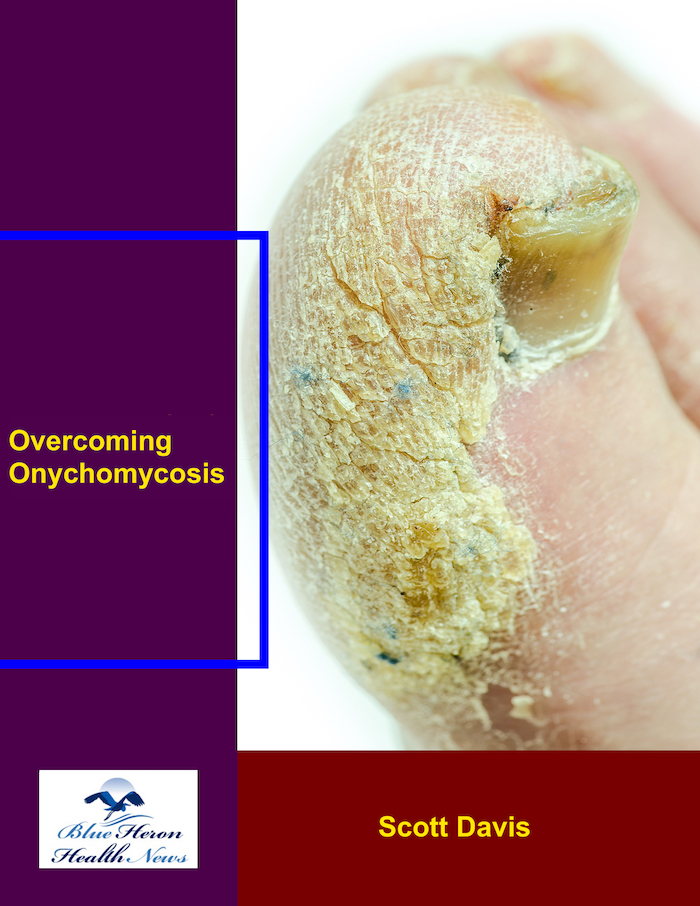
- Onychomycosis:
- Thickened Nails: Infected nails become thickened and difficult to trim.
- Discoloration: Nails may turn yellow, white, brown, or black, depending on the type of fungus. The discoloration usually begins at the edge of the nail and spreads inward.
- Crumbly or Brittle Nails: The nail may become crumbly, flaky, or brittle, and the edges may break easily.
- Distorted Shape: As the infection progresses, the shape of the nail may become irregular or distorted.
- Separation of the Nail: The nail may begin to lift from the nail bed (a condition called onycholysis), leaving a gap where debris can accumulate.
- Foul Odor: In some cases, onychomycosis can produce a slight foul smell.
- Nail Psoriasis:
- Pitting: One of the hallmark symptoms of nail psoriasis is nail pitting, where small, pinprick-like depressions form on the surface of the nails.
- Discoloration: Nails may turn yellow, white, or brown, similar to onychomycosis, but discoloration often appears in oil drop-like patches under the nail, giving a characteristic appearance known as oil-drop sign.
- Thickening of the Nails: Nails may become thickened, though usually not as severely as in onychomycosis.
- Nail Separation: Nails may detach from the nail bed (onycholysis), similar to onychomycosis, but this tends to occur in more advanced stages.
- Ridges and Crumbling: Vertical ridges may form on the nails, and in severe cases, nails can become brittle and crumble.
- Redness and Inflammation: The area around the nail may be red and inflamed, especially if associated with psoriatic arthritis.
3. Location and Association with Other Conditions
- Onychomycosis:
- Primarily affects the toenails but can also affect the fingernails.
- Often associated with athlete’s foot (fungal infection of the skin between the toes) or other fungal skin infections.
- Onychomycosis typically occurs more in older adults and individuals with risk factors such as diabetes, poor circulation, or weakened immune systems.
- Nail Psoriasis:
- Can affect both fingernails and toenails, though fingernails are more commonly involved.
- Usually occurs in individuals with psoriasis and is often accompanied by psoriatic skin lesions on other parts of the body.
- Nail psoriasis is also associated with psoriatic arthritis, where joint inflammation occurs along with nail abnormalities.
4. Diagnosis
- Onychomycosis:
- Nail Clipping or Scraping: Diagnosis is confirmed by taking a sample of the affected nail or nail debris and examining it under a microscope to detect the presence of fungi.
- Culture Test: A fungal culture may be done to identify the specific type of fungus causing the infection.
- PAS Stain: A special stain (periodic acid-Schiff stain) may be used to detect fungal elements in the nail.
- Nail Psoriasis:
- Clinical Examination: Diagnosis is typically based on the appearance of the nails, especially if the patient has a known history of psoriasis or psoriatic skin lesions.
- Exclusion of Infection: A fungal infection must be ruled out if the nail abnormalities are similar to onychomycosis. This may require fungal testing or biopsy to exclude other causes.
5. Treatment
- Onychomycosis:
- Antifungal Medications: Oral antifungal drugs (e.g., terbinafine or itraconazole) are the most effective treatment for onychomycosis, often requiring several months of treatment.
- Topical Antifungal Agents: Topical treatments like ciclopirox or efinaconazole are sometimes used, especially for milder cases, though they may not penetrate the nail deeply enough for severe infections.
- Laser Therapy: Laser treatments are also used in some cases to kill the fungus without harming the surrounding tissues.
- Nail Removal: In severe cases, surgical removal of the infected nail may be required.
- Nail Psoriasis:
- Topical Treatments: Topical corticosteroids, vitamin D analogs (e.g., calcipotriol), and tazarotene are commonly used to reduce inflammation and improve nail appearance.
- Systemic Treatments: In more severe cases, systemic medications such as methotrexate, cyclosporine, or biologic agents (e.g., TNF inhibitors) are used to manage psoriasis and reduce nail involvement.
- Nail Care: Keeping nails short, avoiding trauma to the nails, and using moisturizers can help minimize symptoms.
- Phototherapy: Some patients benefit from ultraviolet light therapy, particularly for psoriatic skin lesions, which may also help with nail symptoms.
6. Prognosis
- Onychomycosis:
- Fungal infections can be difficult to treat, especially if the infection is severe or has affected the nail for a long time. Complete recovery often takes months.
- Onychomycosis can recur, especially in individuals with risk factors like diabetes or poor foot hygiene.
- Nail Psoriasis:
- Nail psoriasis is chronic and can persist throughout life, particularly during psoriasis flare-ups. Treatment helps manage symptoms but may not fully resolve the nail changes.
- Flare-ups may come and go, depending on the severity of the underlying psoriasis and treatment adherence.
7. Contagiousness
- Onychomycosis:
- Contagious: The fungal infection can spread from person to person or through contact with contaminated surfaces like showers, floors, and personal items (e.g., nail clippers, towels).
- Nail Psoriasis:
- Not contagious: Psoriasis, including nail psoriasis, is an autoimmune condition and cannot be transmitted to others.
Conclusion:
The key difference between onychomycosis and nail psoriasis lies in their cause—onychomycosis is a fungal infection that is contagious, while nail psoriasis is an autoimmune condition that is not contagious. While both conditions cause thickened, discolored, and damaged nails, the presence of pitting and psoriatic skin lesions often distinguishes nail psoriasis from onychomycosis. Treatment also differs, with onychomycosis requiring antifungal medications and nail psoriasis often treated with topical or systemic anti-inflammatory agents. Proper diagnosis is essential for effective treatment and management.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!