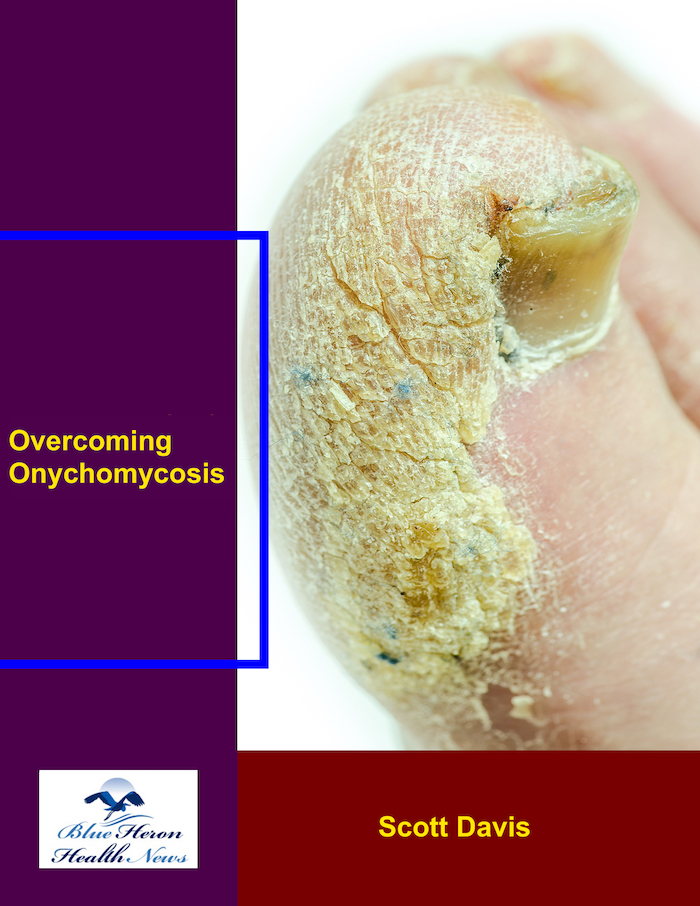
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
How does aging affect the risk of onychomycosis?
Aging is a significant risk factor for onychomycosis, a fungal infection of the nails, due to several physiological and lifestyle changes that occur with advancing age. Here’s a detailed explanation of how aging increases the risk of onychomycosis, supported by multiple sources:
1. Reduced Nail Growth Rate
As people age, the growth rate of nails decreases. Slower nail growth can prolong the exposure of nails to fungi, as the reduced turnover rate allows fungal infections to establish and persist more easily (AAFP).
2. Changes in Nail Structure
Aging often leads to changes in the nail structure, such as increased brittleness and thickening. These changes can create micro-environments that are more conducive to fungal colonization. Brittle nails are more prone to cracks and splits, which can provide entry points for fungal pathogens (AAFP).
3. Compromised Immune Function
The immune system’s efficiency tends to decline with age, a phenomenon known as immunosenescence. This reduced immune function makes it harder for the body to fight off infections, including fungal infections like onychomycosis. Older adults are less capable of mounting a strong immune response to eliminate fungal pathogens (AAFP).
4. Poor Circulation
Many older adults experience reduced blood circulation, particularly to the extremities. Conditions such as peripheral vascular disease and diabetes, which are more common in older populations, further exacerbate poor circulation. This reduced blood flow can impair the delivery of immune cells to the site of infection, making it more difficult to clear fungal infections (AAFP).
5. Increased Risk of Nail Trauma
Aging is often associated with reduced physical dexterity and stability, leading to a higher risk of falls and injuries. Nail trauma, whether from accidental injuries or the cumulative effects of wearing ill-fitting shoes, can damage the nail bed and provide an entry point for fungi (AAFP).
6. Higher Prevalence of Chronic Conditions
Older adults are more likely to have chronic conditions such as diabetes, arthritis, and cardiovascular diseases. These conditions not only increase the risk of developing onychomycosis but also complicate its treatment and management. For instance, diabetic patients often have compromised blood flow and immune function, making them particularly susceptible to fungal infections (AAFP).
7. Increased Use of Communal Facilities
Many older adults live in communal settings such as nursing homes or senior communities, where the use of shared facilities like showers and swimming pools is common. These environments can facilitate the spread of fungal infections, including onychomycosis (AAFP).
Conclusion
The combination of reduced nail growth, changes in nail structure, compromised immune function, poor circulation, increased risk of nail trauma, higher prevalence of chronic conditions, and frequent use of communal facilities makes older adults particularly vulnerable to onychomycosis. Recognizing these risk factors can help in the early detection and management of the condition.
For further reading, you can consult resources such as Mayo Clinic and WebMD.
Can onychomycosis be a sign of an underlying health condition?
Yes, onychomycosis can be a sign of an underlying health condition. The presence of a fungal nail infection may indicate other health issues, particularly those that affect immune function or blood circulation. Here are some common underlying conditions associated with onychomycosis:
**1. **Diabetes
- Increased Susceptibility to Infections: Diabetic patients are at a higher risk for onychomycosis due to several factors, including poor blood circulation, peripheral neuropathy, and a compromised immune system. The high blood sugar levels in diabetes can also create an environment that supports fungal growth (AAFP).
**2. **Immunocompromised States
- Lowered Immune Response: Individuals with weakened immune systems, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or individuals taking immunosuppressive medications, are more susceptible to fungal infections, including onychomycosis. The reduced ability to fight off infections makes these populations particularly vulnerable (AAFP).
**3. **Peripheral Vascular Disease
- Impaired Blood Flow: Conditions that affect blood circulation, such as peripheral arterial disease, can increase the risk of onychomycosis. Poor circulation can lead to reduced oxygen and nutrient delivery to the extremities, impairing the body’s ability to fight infections and heal (AAFP).
**4. **Psoriasis
- Compromised Skin and Nail Integrity: Psoriasis can affect the nails, causing them to thicken, discolor, and become more susceptible to fungal infections. The inflammatory nature of psoriasis can also compromise the skin and nails, making them more prone to infections (AAFP).
**5. **Athlete’s Foot (Tinea Pedis)
- Fungal Spread: Onychomycosis is often associated with athlete’s foot, a fungal infection of the skin of the feet. The fungi can easily spread from the skin to the nails, leading to onychomycosis. This condition is particularly common in individuals who frequently use communal showers or locker rooms (AAFP).
**6. **Other Chronic Conditions
- Rheumatoid Arthritis: Patients with rheumatoid arthritis may be more susceptible to onychomycosis due to their immunosuppressive treatments or reduced mobility, which can lead to poorer foot care and hygiene.
- Obesity: Obesity can contribute to poor circulation and increased sweating, both of which can create a favorable environment for fungal infections (AAFP).
Conclusion
Onychomycosis can be more than just a cosmetic issue; it may be indicative of underlying health conditions that compromise immune function, circulation, or the integrity of the skin and nails. Therefore, the presence of onychomycosis warrants a comprehensive medical evaluation to rule out or manage these associated conditions.
For more detailed information, you can refer to sources like Mayo Clinic and WebMD.
How does diabetes influence the risk of onychomycosis?
Diabetes significantly increases the risk of developing onychomycosis, a fungal infection of the nails. Several factors associated with diabetes contribute to this heightened risk:
1. Compromised Immune System
Diabetic individuals often experience a compromised immune system, which impairs the body’s ability to fight off infections, including fungal infections like onychomycosis. High blood sugar levels can weaken immune responses, making it easier for fungi to establish and spread in the nails (AAFP).
2. Poor Blood Circulation
Diabetes can lead to poor blood circulation, particularly in the extremities (hands and feet), a condition known as peripheral vascular disease. Reduced blood flow can slow down the delivery of immune cells and nutrients necessary for maintaining healthy nails and fighting infections. This poor circulation can also lead to a higher incidence of minor injuries or trauma to the nails, providing entry points for fungi (AAFP).
3. Neuropathy
Peripheral neuropathy, a common complication of diabetes, results in decreased sensation in the extremities. This reduced sensation can prevent individuals from noticing minor injuries or infections in the nails and feet. These unnoticed injuries can become entry points for fungi, increasing the risk of onychomycosis (AAFP).
4. Elevated Blood Sugar Levels
High blood glucose levels create an environment conducive to fungal growth. The excess sugar in the blood can promote the growth of fungi, including those that cause onychomycosis. This is particularly problematic in diabetic patients, who often have difficulty regulating blood sugar levels effectively (AAFP).
5. Higher Incidence of Other Fungal Infections
Diabetic patients are more susceptible to other fungal infections, such as athlete’s foot (tinea pedis). These infections can easily spread to the nails, leading to onychomycosis. The presence of one fungal infection can increase the likelihood of another, compounding the risk (AAFP).
Prevention and Management
To prevent and manage onychomycosis, diabetic patients should:
- Maintain good blood sugar control.
- Practice good foot hygiene, including regular washing and thorough drying of the feet.
- Avoid walking barefoot in communal areas.
- Inspect their feet and nails regularly for signs of infection or injury.
- Consult healthcare providers promptly if they notice any changes in their nails or feet.
For more detailed information, refer to resources such as the Mayo Clinic and American Academy of Dermatology.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!