Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is total dystrophic onychomycosis?
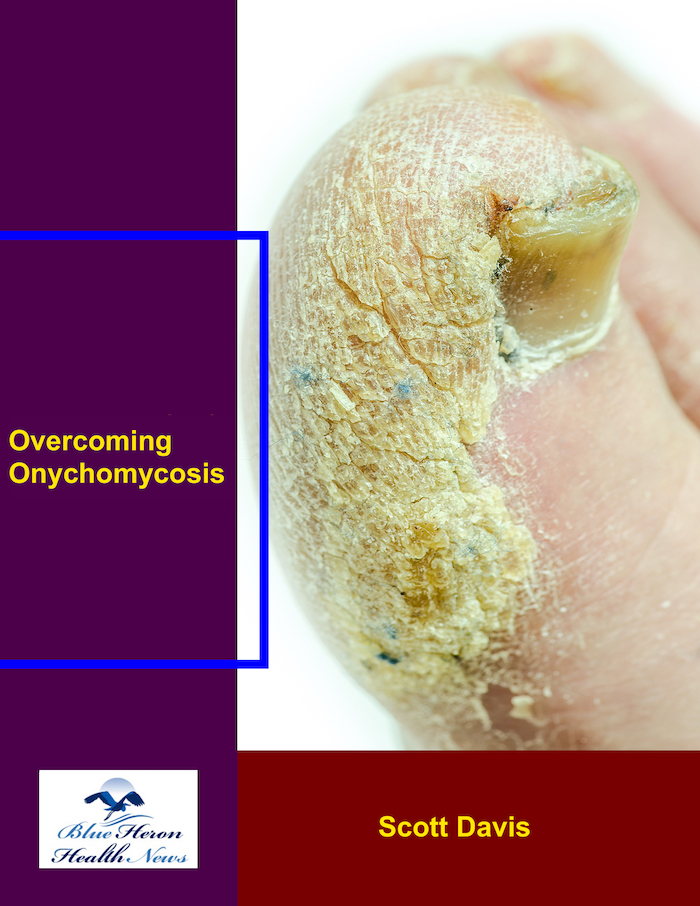
Total dystrophic onychomycosis (TDO) is the most severe form of onychomycosis, characterized by extensive nail damage and dysfunction. It typically represents the end stage of untreated or inadequately treated fungal nail infections, where the infection has progressed to involve the entire nail unit, including the nail plate, bed, and matrix. TDO can affect both fingernails and toenails, though it is more commonly seen in toenails due to factors like moisture and pressure from footwear.
Key Characteristics and Symptoms
- Complete Nail Destruction:
- In TDO, the nail plate is often completely destroyed, leaving little to no normal nail structure. The nail may appear thickened, brittle, and crumbly, often disintegrating or breaking away.
- Severe Nail Discoloration:
- The affected nails can exhibit significant discoloration, ranging from white to yellow, brown, or even black, depending on the type of fungi and the presence of secondary bacterial infections.
- Onycholysis and Subungual Debris:
- Onycholysis, or the detachment of the nail from the nail bed, is a common feature. This detachment allows for the accumulation of fungal debris, keratin, and other materials under the nail, contributing to a rough and uneven nail surface.
- Nail Thickening and Deformation:
- The nails may become severely thickened (subungual hyperkeratosis) and deformed. The shape of the nails can become distorted, often with a rough, bumpy surface.
- Pain and Discomfort:
- TDO can be painful, particularly when the thickened and deformed nails press against the surrounding skin or when secondary bacterial infections occur. The pain may be exacerbated by pressure from shoes or other external factors.
- Secondary Infections:
- The damaged nail structure can create a favorable environment for bacterial infections, further complicating the condition and potentially leading to cellulitis or other skin infections.
Causes
Total dystrophic onychomycosis is caused by prolonged and severe fungal infections. The fungi responsible are usually dermatophytes, with Trichophyton rubrum being the most common pathogen. However, other fungi, including non-dermatophyte molds and yeasts like Candida, can also contribute, especially in immunocompromised individuals.
Risk Factors
- Chronicity of Infection:
- TDO often develops after long-standing, untreated, or poorly treated nail infections. The chronic nature of the infection allows the fungi to progressively damage the nail unit.
- Immunocompromised Conditions:
- Individuals with weakened immune systems, such as those with HIV/AIDS, diabetes, or undergoing chemotherapy, are at higher risk for developing TDO.
- Trauma and Poor Circulation:
- Nail trauma and poor circulation, common in older adults and individuals with peripheral vascular disease, can predispose to more severe forms of onychomycosis.
Diagnosis
Diagnosing TDO involves a thorough clinical examination and laboratory tests, such as:
- KOH Preparation: To identify fungal elements in nail samples.
- Fungal Culture: To determine the specific type of fungus causing the infection.
- PCR Testing: For rapid and precise identification of fungal DNA.
These diagnostic tools are essential for confirming the diagnosis and guiding treatment decisions.
Treatment
Treating total dystrophic onychomycosis can be challenging due to the extensive nail damage and the involvement of the nail matrix. Treatment options include:
- Oral Antifungal Medications:
- Oral antifungals like terbinafine, itraconazole, or fluconazole are often required. The treatment course may be long, typically several months, to ensure complete eradication of the infection.
- Topical Antifungal Agents:
- While less effective as monotherapy in TDO, topical treatments may be used in conjunction with oral medications.
- Nail Removal:
- Surgical or chemical removal of the affected nail may be necessary, particularly if the nail is causing pain or if topical and oral treatments are insufficient.
- Laser Therapy:
- Laser treatments may be considered as an adjunctive therapy to target and destroy fungal elements within the nail.
- Prevention and Management of Secondary Infections:
- Proper care and hygiene, along with potential antibiotic treatment, are important to prevent and manage secondary bacterial infections.
References:
- Mayo Clinic Nail Fungus (Onychomycosis)
- American Academy of Dermatology Onychomycosis Overview
Total dystrophic onychomycosis requires comprehensive treatment and management to address the extensive nail damage and prevent further complications. Early intervention and adherence to treatment are crucial for achieving the best outcomes.
How common is onychomycosis?
Onychomycosis is a relatively common condition, affecting a significant portion of the population worldwide. The prevalence of onychomycosis varies depending on factors such as age, geographical location, and underlying health conditions.
Prevalence and Demographics
- General Population:
- The prevalence of onychomycosis in the general population is estimated to be around 10% globally. This prevalence can vary widely, with reports ranging from 2% to 18% depending on the region and study population (AAFP).
- Age Factors:
- Onychomycosis is more common in older adults. Studies indicate that the prevalence increases with age, affecting up to 20-30% of individuals over the age of 60. This increased prevalence is due to factors such as reduced nail growth rate, diminished immune response, and a higher likelihood of chronic health conditions (AAFP).
- Geographical Variation:
- The prevalence of onychomycosis also varies geographically. Higher rates are often reported in countries with warmer and more humid climates, which are conducive to fungal growth. For example, prevalence rates in tropical and subtropical regions can be significantly higher compared to temperate regions (AAFP).
- Underlying Health Conditions:
- Certain health conditions, such as diabetes, peripheral vascular disease, and immunosuppressive disorders (e.g., HIV/AIDS), are associated with a higher prevalence of onychomycosis. Diabetic patients, for instance, are particularly prone to fungal infections due to compromised blood circulation and immune response (AAFP).
- Gender Differences:
- Some studies suggest that men may be slightly more affected by onychomycosis than women, although the difference is not substantial. This could be due to differences in nail care practices, occupational exposures, and footwear habits (AAFP).
Conclusion
Onychomycosis is a common nail disorder, affecting millions of people globally. The condition’s prevalence is influenced by age, geographical location, and underlying health conditions. Early diagnosis and treatment are essential to manage the infection effectively and prevent complications.
For more detailed information, refer to sources such as WebMD and the American Academy of Dermatology.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!