Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
How is onychomycosis diagnosed?
Diagnosing onychomycosis, a fungal infection of the nails, involves a combination of clinical assessment and laboratory tests. The diagnosis process is crucial because the symptoms of onychomycosis can be similar to those of other nail conditions, such as psoriasis, lichen planus, or trauma-induced changes. Here’s a detailed overview of the diagnostic process for onychomycosis:
1. Clinical Evaluation
Visual Inspection:
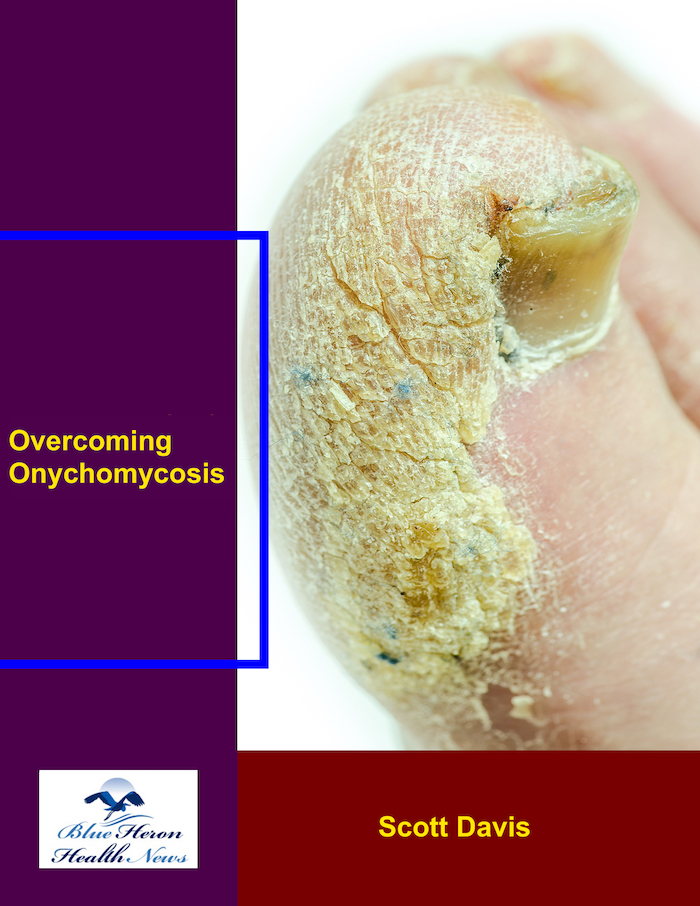
- The initial step in diagnosing onychomycosis involves a thorough clinical evaluation by a healthcare provider. This includes a visual inspection of the affected nails and surrounding skin to assess the extent and characteristics of the infection. Key features examined include nail discoloration, thickening, brittleness, separation from the nail bed (onycholysis), and any associated pain or discomfort.
History Taking:
- A detailed medical history is taken to identify any risk factors, such as a history of fungal infections, diabetes, immunosuppressive conditions, family history of onychomycosis, or lifestyle factors like frequent use of communal showers or nail salons.
2. Laboratory Tests
Given the similarity in appearance between onychomycosis and other nail disorders, laboratory confirmation is often necessary to establish an accurate diagnosis. The main laboratory methods include:
A. Potassium Hydroxide (KOH) Preparation:
- A KOH preparation is a simple and quick test to detect fungal elements. During this test, a small sample of the affected nail or nail debris is scraped off and placed on a microscope slide. Potassium hydroxide solution is then added, which dissolves the keratin in the sample, making it easier to see fungal elements under a microscope. The presence of branching hyphae (fungal filaments) or spores can confirm a fungal infection (AAFP).
B. Fungal Culture:
- Fungal culture involves growing the nail sample on a specialized medium to identify the specific fungus causing the infection. This method is more definitive than a KOH test but takes longer (several weeks) to yield results. It can identify the exact species of fungus, including dermatophytes, non-dermatophyte molds, and yeasts like Candida. This information can be critical for selecting the most appropriate treatment (AAFP).
C. Nail Biopsy and Histopathology:
- In some cases, a nail biopsy may be performed, where a small piece of the affected nail or nail bed is removed for histopathological examination. This can provide detailed information about the extent of fungal invasion and any associated inflammatory response. This method is particularly useful when the diagnosis is uncertain or when differentiating onychomycosis from other conditions like psoriasis or lichen planus (AAFP).
D. Polymerase Chain Reaction (PCR) Testing:
- PCR testing is a molecular diagnostic technique that detects fungal DNA in nail samples. It is highly sensitive and can provide rapid results, identifying the fungal species present. While not routinely used due to cost and availability, PCR can be particularly useful in complex cases or when previous tests have been inconclusive (AAFP).
Differential Diagnosis
Excluding Other Conditions:
- The differential diagnosis of onychomycosis involves distinguishing it from other conditions that can cause similar nail changes. These include:
- Psoriasis: Can cause pitting, discoloration, and thickening of the nails.
- Eczema: Can lead to nail ridging and thickening.
- Trauma: Repeated nail injury can mimic fungal infection symptoms.
- Lichen Planus: Can cause nail ridging and thinning.
- Alopecia Areata: May present with nail pitting and discoloration.
Conclusion
Accurate diagnosis of onychomycosis requires a combination of clinical assessment and laboratory testing. While visual inspection and patient history are essential first steps, laboratory confirmation through KOH preparation, fungal culture, nail biopsy, or PCR testing is often necessary to confirm the diagnosis and guide appropriate treatment. Differentiating onychomycosis from other nail conditions is crucial for effective management and treatment.
For more detailed information, you can consult resources such as Mayo Clinic and American Academy of Dermatology.
What types of fungi commonly cause onychomycosis?
Onychomycosis, a fungal infection of the nails, can be caused by various types of fungi. The most common types of fungi that cause onychomycosis are dermatophytes, yeasts, and non-dermatophyte molds. Here’s a detailed breakdown of these fungal types:
1. Dermatophytes
Dermatophytes are the most common cause of onychomycosis, particularly in toenails. They are specialized fungi that thrive on keratin, a protein found in nails, skin, and hair. The most prevalent dermatophyte species include:
- Trichophyton rubrum: The leading cause of onychomycosis, this species primarily affects the toenails but can also infect fingernails. It often causes distal subungual onychomycosis, characterized by yellow discoloration, thickening, and nail separation from the bed.
- Trichophyton mentagrophytes: The second most common dermatophyte, responsible for a significant number of toenail infections. It can cause similar symptoms to T. rubrum but is sometimes associated with more inflammation.
- Epidermophyton floccosum: Although less common, this dermatophyte can also cause nail infections, particularly in warmer climates.
2. Yeasts
Yeasts, especially from the genus Candida, can cause onychomycosis, predominantly in fingernails. Yeast infections are more common in individuals with compromised immune systems or those exposed to frequent moisture. Key species include:
- Candida albicans: The most common yeast causing onychomycosis, often leading to whitish or yellowish nail discoloration, thickening, and onycholysis. It is more likely to affect fingernails and can cause chronic paronychia (inflammation of the nail folds).
- Candida parapsilosis and Candida tropicalis: Other species that may cause nail infections, particularly in immunocompromised patients.
3. Non-Dermatophyte Molds
Non-dermatophyte molds are less common causes of onychomycosis but can still lead to nail infections, especially in nails that have been previously damaged. These fungi include:
- Scopulariopsis brevicaulis: Often causes superficial white onychomycosis, presenting with white, chalky patches on the nail surface.
- Fusarium species: Known for causing a wide range of infections, Fusarium can lead to onychomycosis characterized by nail discoloration, thickening, and potential nail detachment.
- Aspergillus species: These molds are more commonly associated with respiratory infections but can also cause nail infections, particularly in immunocompromised individuals.
- Acremonium species: Another group of molds that can infect nails, often resulting in a similar appearance to dermatophyte infections.
Mixed Infections
In some cases, onychomycosis can involve mixed infections, where more than one type of fungus is present. This can complicate diagnosis and treatment, as different fungi may require different antifungal therapies.
Conclusion
Understanding the specific type of fungus causing onychomycosis is crucial for effective treatment. Dermatophytes, yeasts, and non-dermatophyte molds each have different susceptibilities to antifungal agents, making accurate identification essential. Laboratory testing, such as culture or molecular methods, can help determine the exact cause and guide appropriate treatment.
For more detailed information, you can refer to resources like the Mayo Clinic and American Academy of Dermatology.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!