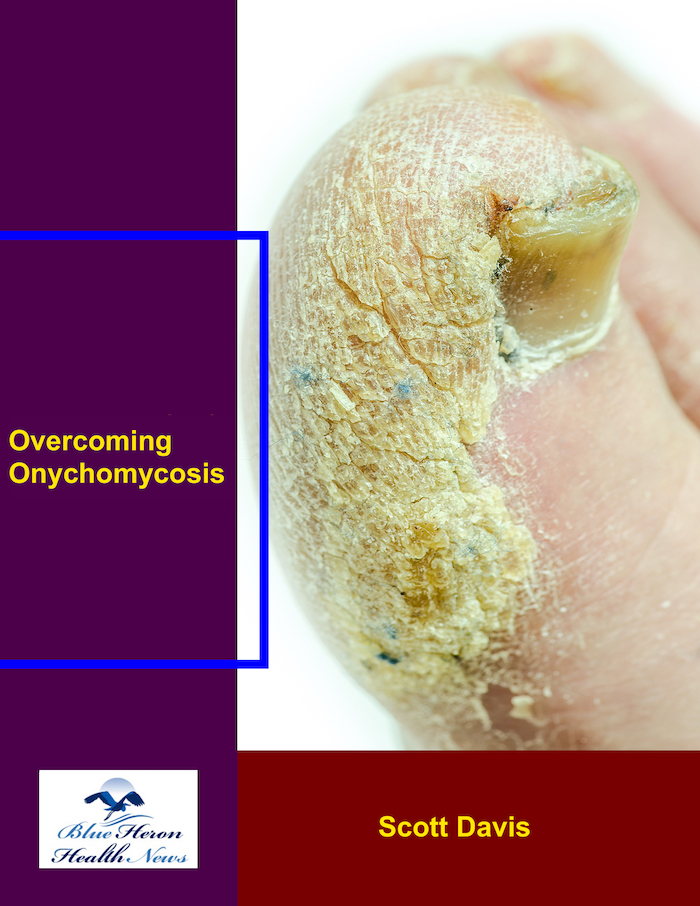
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What are the treatment options for distal subungual onychomycosis?
Distal subungual onychomycosis (DSO) is the most common form of onychomycosis, a fungal infection of the toenails or fingernails. It starts at the distal (tip) edge of the nail and progresses toward the nail base, leading to thickening, discoloration, and separation of the nail from the nail bed. Treatment of DSO is directed towards the elimination of the fungal infection, improvement in the appearance of the nail, and prevention of recurrence.
Treatment of Distal Subungual Onychomycosis
1. Topical preparations containing antifungals
Mild to moderate DSO can typically be treated with a topical antifungal, especially when only part of the nail is affected. Topical antifungals destroy the fungus or inhibit the growth of the fungus.
Common topical treatments are:
Ciclopirox (Penlac Nail Lacquer): This lacquer antifungal is placed directly on the infected nail and the surrounding skin. It is applied once daily for several months at a time.
Amorolfine (Loceryl): Antifungal nail lacquer applied to the infected nail and may be useful in mild DSO.
Terbinafine (Lamisil) cream or gel: Applied topically from time to time for mild or superficial infections.
Efinaconazole (Jublia): Newer topical antifungal solution applied to the affected nail, typically once daily for 48 weeks. Useful in mild to moderate DSO.
Benefits of topical treatments:
Easier to apply
Less likelihood of side effects
Effective in the initial infection stages
Disadvantages:
Less effective in large or severe infections
Must be applied regularly for months
Can be hard to apply to thickened nails
2. Oral Antifungal Drugs
Oral antifungals are more commonly employed in serious or big cases of DSO, especially if the topicals fail.
Common oral antifungal drugs are:
Terbinafine (Lamisil): Widely utilized as the first-line oral therapy for onychomycosis. Most often prescribed for 6-12 weeks, it inhibits fungal cell wall formation. It is highly effective but may require monitoring of liver function due to concomitant side effects.
Itraconazole (Sporanox): Another oral antifungal that can be used for more serious cases of DSO. It is usually taken in pulse therapy (e.g., one week of treatment, followed by a week off), which can lengthen the overall treatment time.
Fluconazole (Diflucan): An oral antifungal alternative that can be effective against fungal nail infections but is not as commonly used as terbinafine or itraconazole.
Advantages of oral treatments
More effective in cases of severe or widespread infections
Faster results compared to topical treatment
Limitations:
Side effects risk, including liver toxicity, drug interaction, and gastrointestinal upset
Needs prescription and potentially includes monitoring side effects
More time required for treatment, typically 6-12 weeks
3. Debridement and Trimming of the Nail
Debridement of the nail is the mechanical removal of infected nail tissue to reduce the burden of the fungus. It may be done by a health practitioner or podiatrist.
Normal nail trimming can help to thin the nail so that topical therapy is more easily absorbed.
Advantages:
Enhances the aesthetic appeal of the nail
Reduces pain and pressure of thickened nails
Disadvantages:
Treats the symptom (thickness, pain) but not the underlying fungus infection
Must be combined with antifungal therapy for complete resolution
4. Laser Therapy
Laser treatment uses a focused light to kill the fungi within the infected nail. 1064 nm Nd:YAG laser is among the lasers used in the treatment of onychomycosis, and it is utilized to penetrate the nail and kill the fungus beneath.
Advantages:
Non-invasive
Fairly quick treatment with minimal downtime
No systemic side effects
Disadvantages:
It may require multiple sessions
May not be covered by insurance
Results will vary, and effectiveness will depend on infection severity
5. Combination Treatment
Combination treatment (oral and local treatments) is used in most cases to achieve maximum results. This treatment can help treat the infection more effectively by acting on different regions of the fungus and improving overall penetration.
For example, an oral antifungal like terbinafine can be paired with a topical treatment like ciclopirox or amorolfine.
Advantages:
Enhances the possibility of eradicating the infection
Topical medications can reduce the need for prolonged oral treatment
Disadvantages:
Enhances the complexity of the treatment regimen
May increase the possibility of side effects due to oral treatment
Preventive Measures
Proper hygiene of the feet: Keeping the feet clean and dry, especially between the toes, can prevent fungal infection.
Avoiding the sharing of footwear: Fungal infections are transmitted by infected surfaces or through sharing footwear.
With antifungal sprays or powders: Daily application of antifungal solutions to the feet or nails can reduce the risk of developing an infection, especially in people with frequent infections.
Conclusion
DSO treatment typically involves antifungal agents, whether topical or oral, and nail debridement or laser therapy for severe cases. The mode of treatment will depend on the severity of the infection, the number of affected nails, and the overall health of the patient. If you think you have DSO, it is best to consult a healthcare provider or a dermatologist to decide on a treatment plan.
White Superficial Onychomycosis (WSO) is a fungal infection in the surface layer of the nail that whitens and powders or chalks the nail. It is not as severe as other onychomycosis conditions but has to be still diagnosed and treated accordingly. These are the ways WSO should be diagnosed:
1. Clinical Examination:
Visual Inspection: The first component of the diagnosis of WSO is an exhaustive clinical inspection of the nails. Affected nails typically have white, opaque, or chalky patches on the surface of the nail plate. Such patches are either localized to the nail surface or spread to the nail.
Location: The infection most often occurs on the dorsal (top) surface of the nails and is seen as patchy, white lesions that tend to spread progressively. It is most commonly found on toenails but may affect fingernails.
No Involvement of Nail Bed or Matrix: Unlike other forms of onychomycosis, WSO does not involve the nail bed or nail matrix, so the nail plate is intact or relatively so beneath the surface.
2. KOH (Potassium Hydroxide) Preparation
Nail Scraping: Infected nail material is scraped from the skin surface of the lesion. A bit of it is placed on a glass slide and treated with potassium hydroxide (KOH).
Microscopic Examination: Microscopically, evidence of fungal elements such as hyphae or spores confirms WSO diagnosis. KOH preparation breaks down non-fungal components so that fungal elements are better seen.
3. Fungal Culture
Nail Culture: Nail culture may be done for fungal culture to identify the causative organism of infection. The most frequent causative organisms for WSO are dermatophytes, among which Trichophyton mentagrophytes or Trichophyton rubrum.
Identification of Causative Organism: Fungal culture can help in identifying the specific causative organism, which can help in deciding on appropriate treatment.
4. Wood’s Lamp Examination
A Wood’s lamp (a special form of ultraviolet light) may be used, on occasion, to view fungal infections, but this examination is more commonly used to detect fungal skin infection, rather than nail infection. Fungal infections may, on rare occasions, fluoresce yellow-green using the lamp.
It’s not the optimum test for diagnosis of WSO, however, and it’s more commonly used for skin infection like tinea versicolor.
5. Nail Biopsy:
In rare circumstances, if the diagnosis is suspicious or if the infection is failing to respond to standard treatments, a nail biopsy may be performed. A minor portion of the nail is removed and analyzed for histopathological examination to determine the presence of fungal infection.
Biopsy is usually performed only when the diagnosis is uncertain or if other diseases need to be ruled out.
6. Differential Diagnosis:
The doctor will also consider other conditions that have a similar appearance to WSO, such as:
Psoriasis: Psoriasis can lead to nail changes like pitting, color alteration, and thickening, which might have a resemblance to WSO.
Trauma: There can be white spots or color alteration from physical trauma to the nail that could be confused with WSO.
Eczema or Dermatitis: Involvement of the nail in skin diseases may result in color alteration or surface changes that look like WSO.
Conclusion
Diagnosis of White Superficial Onychomycosis (WSO) is accomplished through a combination of clinical observation, microscopic inspection with KOH preparation, and culture to reveal fungal structures and establish the causative organism. The diagnosis is aimed at ensuring precise diagnosis and appropriate treatment for the infection.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!