Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is total dystrophic onychomycosis?
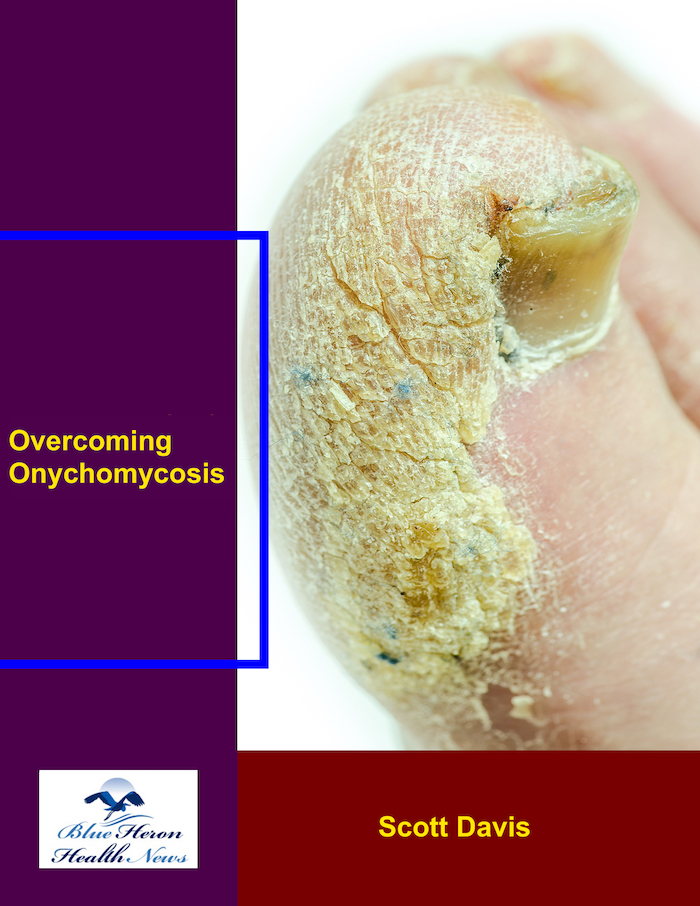
Total dystrophic onychomycosis (TDO) is a severe nail fungus (onychomycosis) that leads to extensive damage and deformation of the affected nails. In TDO, the fungus infects the entire nail, typically causing the nail to become thickened, discolored, crumbling, and detached from the nailbed. “Dystrophic” refers to the degeneration or deterioration of the nail.
Key Features of Total Dystrophic Onychomycosis:
Extensive Nail Involvement:
TDO encompasses the whole nail, both the nail plate and nailbed. It is the most severe stage of onychomycosis, with the fungal infection penetrating deeply into the nail tissue.
Nail Deformation:
The nails become thick, deformed, and fissured. The nail loses its natural form, and the affected portion of the nail is deformed.
The nail plate may be separated from the nailbed (a process known as onycholysis), with additional damage and possible complete loss of the nail.
Discoloration:
The infected nail may turn yellow, brown, white, or greenish, depending on the fungal agent involved in the infection. Discoloration can cover the entire nail.
Nail can become opaque or cloudy in certain cases.
Debris Under the Nail:
A build-up of fungal debris and keratin may occur beneath the nail plate, which can thicken and pigment the nail.
It may also have an offensive smell due to the accumulation of fungal material.
Pain and Tenderness
The infected nails may become sensitive or painful, especially if nail lifting or trauma is induced by the fungal infection. In severe cases, there may be pressure sensitivity or failure to wear shoes in the event of toenail infection.
Nail Loss:
In the most advanced cases, TDO can result in nail loss. The nail may come off from the nailbed completely, causing permanent damage to the nail structure.
Cause:
TDO is usually caused by dermatophytes, which are fungi that infest hair, nails, and skin. Trichophyton rubrum and Trichophyton mentagrophytes are the most common species that produce TDO.
Other fungi, such as Candida species, may also be the cause in people with immunocompromised states or diabetes.
Untreated or chronic onychomycosis may result in the production of TDO.
Risk Factors:
Chronic fungal infections: Chronic fungal infections or untreated onychomycosis can progress to TDO.
Immunocompromised states: Those with weakened immune systems, for instance, patients with HIV/AIDS, diabetes, or those who are undergoing chemotherapy, are at a greater risk of developing TDO.
Poor circulation: Conditions like peripheral artery disease or diabetes can hinder the body from being able to eliminate fungal infections, resulting in TDO.
Nail trauma: Trauma to the nail or chronic nail trauma to the area can provide a portal of entry for the fungus to infiltrate deeper within the nail plate.
Diagnosis:
Diagnosis is most commonly made on a clinical basis, with the classical presentations of nail thickening, discoloration, and deformity being diagnosed.
Microscopic examination or culture of infected nail clippings may be necessary to confirm fungal presence and to identify the etiologic agent.
Treatment
Oral antifungal agents: Since TDO is a full-nail infection and has a propensity to extend into the nail bed, oral antifungal treatment is generally required. Medications like terbinafine, itraconazole, and fluconazole are most often used.
Topical antifungals: In conjunction with oral medications, topical antifungal treatment in the form of ciclopirox nail lacquer, for instance, may be used, but it is generally not as effective for severe infections like TDO.
Nail debridement: Trimming of the nail and removal of the infected nail, or nail surgery, may be necessary in severe cases to reduce the fungal load and allow topical therapy to penetrate better.
Laser therapy: Laser therapy, which kills the fungal cells under the nail, may be beneficial for some patients.
Prevention:
Good hygiene: Keeping hands or feet dry and clean helps prevent fungal infection. Frequent changing of socks and not wearing tight, wet shoes can prevent onychomycosis.
Not using public showers or pools: Wearing sandals in communal wet areas (such as pools or gyms) can prevent fungal infection.
Treatment of underlying conditions: Controlling diseases such as diabetes and enhancing immune system function can help prevent fungal infection.
Nail care: prevention of trauma and injury to the nails is essential to prevent entry of fungus.
Conclusion:
Total dystrophic onychomycosis is a severe and advanced nail fungus infection, which can result in extensive damage to the nail such as thickening, pigmentation, and even loss of the nail. It is most commonly caused by dermatophytes or Candida, particularly in those with compromised immunity or chronic fungal infection. Treatment is normally oral antifungal therapy, topical therapy, and in some cases, debridement or laser treatment of the nails. Prevention, however, involves cleanliness and protection of the nails against infection.
You are welcome to ask more about onychomycosis prevention and treatment!
Distal subungual onychomycosis (DSO) is the most common form of onychomycosis (nail fungal infection), where it affects the distal (tip) portion of the nail, typically starting at the free edge of the nail and progressing toward the nail bed. It typically is caused by dermatophytes, specifically the Trichophyton rubrum species, but can be caused by other forms of fungi such as Trichophyton mentagrophytes.
Development of Distal Subungual Onychomycosis (DSO):
Initial Infection
The infection usually starts at the distal (loose) end of the nail and then progresses proximally (towards the nail bed).
Symptoms in initial stages are white or yellowish discoloration at the tip of the nail, initially mild.
Thickening and Crumbling:
As the infection proceeds, the infected area thickens and the nail begins to crumble or become cloudy.
The nail plate becomes weak and brittle, and the infection progresses further towards the base of the nail.
The nail may also become deformed, with ridges or striations in a longitudinal direction.
Subungual Hyperkeratosis:
As the fungal infection reaches deeper layers of the nail plate, it may infect the nail bed and cause subungual hyperkeratosis (thickening of the skin of the nail bed).
This thickening can be painful or sore if the nail also becomes lifted from the nail bed.
Separation from the Nail Bed (Onycholysis):
Later, as the infection continues, the infected portion of the nail can begin to peel away from the nail bed (a term known as onycholysis). It can create space between the nail and the nail bed, thereby allowing more fungus growth and an intensification of the infection.
The nail started loosening and may or may not fall off or need to be dislodged due to severe damage.
Discoloration and Debris:
The infected nail will become discolored, typically yellow or brown, or greenish in hue as the fungus advances and becomes more embedded into layers.
Fungal debris and keratin of the nail plate tend to accumulate underneath, which may create a crumbly or powdery feel.
The nail will also provide a foul-smelling discharge due to the fungal infection and necrotic debris accumulation.
Chronic Stage:
Distal subungual onychomycosis becomes chronic, if left untreated for a few months or years.
Infection may spread and extend to more than one nail, with progressive extension and increase of the process.
Deformation of nails due to infection may also occur along with chronic damage to the nail matrix so that life-long nail conditions could be anticipated to ensue.
Possible Complications:
Discomfort and pain: As the infection swells and results in nail thickening or elevation, this may be followed by pain or tenderness, particularly on pressure or tight pressure due to wearing tight shoes.
Secondary infections: Since the infection also results in detachment of the nail from the nail bed (onycholysis), the possibility of developing bacterial infections or other complications may be greater.
Infection spread: The fungal infection may spread to the other nails or parts of the body, particularly if not treated for prolonged periods.
Deformation of the nail: Long-term DSO may cause permanent nail deformation, which can be difficult to correct even after successful eradication of the fungal infection.
Treatment Options:
Topical Antifungals:
Ciclopirox nail lacquer or amorolfine are the commonly used topical drugs applied locally on the infected nail.
Treatment will typically take a few months to be effective because the nail must grow back fully before the infection is gone.
Milder infections or where there is minimal nail involvement may be treated with topical antifungals.
Oral Antifungal Medicines:
Terbinafine, itraconazole, and fluconazole are the most frequently prescribed oral antifungals for more severe or extensive infections.
Oral therapy is typically indicated for large DSO or where local therapy has failed, and treatment is typically 6 to 12 weeks in duration.
The drugs do have potential side effects, and monitoring during therapy is thus warranted.
Nail Debridement:
Debridement of the nail (surgical cutting, filing, or sanding of infected nail) can be performed to remove infected tissue and reduce fungal load.
This can be done by a health professional or at home with the correct gear.
This contributes to the reinforcement of local treatment and might provide symptomatic alleviation.
Laser Therapy:
Laser therapies (such as Nd:YAG laser) have been found to assist with the treatment of onychomycosis through the use of light energy applied to the diseased tissue.
This treatment can be effective for resistant cases of topical and oral medication, although it tends to be more expensive and can require being performed in multiple sessions.
Preventative Actions:
Regular nail cleaning and drying must be accomplished to prevent further fungus growth.
Proper foot hygiene, wearing well-ventilated shoes, and not sharing nail clippers or shoes can help prevent reinfection.
In some cases, antifungal creams are used preventively topically, especially on those who are prone to recurrent infections.
Prognosis:
Early treatment of distal subungual onychomycosis that is successful typically has a good outcome, and the nail will eventually grow back normally since the fungal infection is eradicated.
Since nails grow slowly, however, it may be many months before the improvements become evident even with effective treatment.
In advanced or chronic cases, matrix structural damage will result in long-term nail deformity or more prolonged treatment courses.
If you require further information regarding onychomycosis treatment or treatment options, we can let you know!
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!