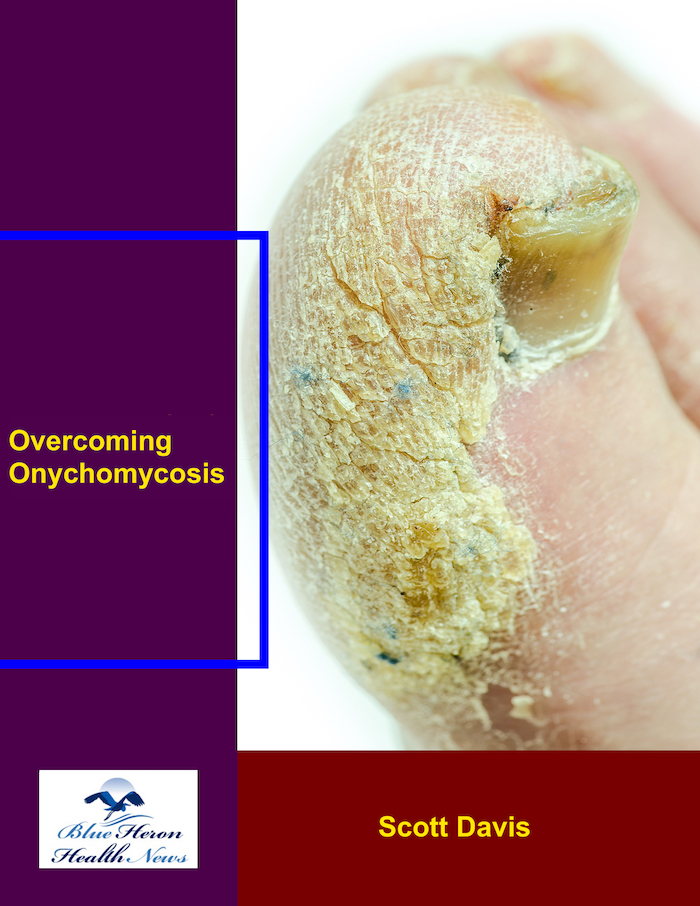
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is proximal subungual onychomycosis?
Proximal subungual onychomycosis (PSO) is a type of nail fungus infection (onychomycosis) in the proximal (base) region of the nail, where the cuticle and nail meet. PSO is less common than distal subungual onychomycosis (DSO), but it is an important variant to know.
Important Features of Proximal Subungual Onychomycosis:
Location:
The infection starts at the base of the nail (proximal aspect), often where the cuticle is or where the nail bed is, and progresses to the free edge of the nail.
It primarily attacks the nailbed beneath the nail plate, with the fungal infection spreading from the base of the nail.
Appearance:
The affected nail typically becomes discolored (typically white or yellow), typically in the area of the cuticle.
White or yellow lines may form along the nail plate, starting at the base and running to the tip.
As the infection progresses, the nail may become thickened, deformed, or crumbly.
In some cases, there is detachment of the nail from the nailbed (onycholysis), typically at the proximal part of the nail.
Causes:
Dermatophytes (fungi that most commonly infect hair, skin, and nails) are the most common cause, namely Trichophyton rubrum and Trichophyton mentagrophytes species.
Candida species (yeast) can also cause proximal onychomycosis, particularly in patients with compromised immune systems, nail trauma, or frequent exposure to water (e.g., frequent hand washing).
Trauma to the nail or cuticle area can increase the chances of invasion by fungi and infection.
Risk Factors
Immunocompromised: People with compromised immune systems (e.g., HIV/AIDS, diabetes, chemotherapy, or steroid use) have a higher likelihood of contracting PSO.
Trauma to the nail: Trauma to the nail, especially in the region of the cuticle, offers more opportunity for fungal invasion.
Exposure to dampness: Repeated exposure to damp environments or persistent dampness (e.g., wet gloves, overwashing of hands) provides an environment conducive to the development of fungi.
Poor circulation: Conditions that affect blood flow (like peripheral artery disease) can make it harder for the immune system to fight infections.
Fungal infections elsewhere: If there is a history of fungal infections of the skin or other fungal nail infections, there is an increased risk for PSO.
Symptoms:
Discoloration: The nail may turn white, yellow, or brown at the base and become discolored with the development of the infection.
Thickening of the nail: The nail may become thicker and more difficult to cut as the infection advances.
Deformation of the nail: The nail may grow deformed in shape as the fungus is damaging the nail plate and nailbed.
Pain or soreness: The infected nail can become painful, especially on putting pressure on the underside of the nail.
Separation of the nail: In more severe cases, the nail itself may be separated from the nailbed, resulting in onycholysis (nail lifting).
Diagnosis:
Clinical examination: A healthcare provider usually diagnoses PSO based on the characteristic appearance of the nail and where it is positioned at the proximal region of the nail.
Lab diagnosis: To make the diagnosis and ascertain the correct fungus, an infected nail may be sampled to do a microscopic examination, culture of the fungus, or PCR.
Treatment:
Topical antifungal agents: Antifungal creams, ointment, or lacquer (like ciclopirox nail lacquer) may succeed, but for it to take effect, there might need to be prolonged treatment and is successful in early presentation or for diseases limited to superficial infection.
Oral antifungal medications: In more severe or disseminated infections, terbinafine, itraconazole, or fluconazole may be used to cure the fungal infection from the inside out.
Nail debridement: Chopping and removing the infected areas of the nail might allow antifungal medication to penetrate better and might provide relief.
Laser treatment: Laser treatment can sometimes be used to cure the fungal infection by killing and destroying the fungus beneath the nail.
Prevention:
Good hygiene: Keeping the nails and cuticles as clean and dry as possible is crucial to preventing fungal infection. Moisture should be prevented, and nails should be trimmed regularly.
Preventing trauma: Protecting the nails from harm, particularly around the area of the cuticle, can reduce the risk of fungal penetration.
Minimizing exposure to wet communal areas: Swims or water shoes worn by the public in such areas as pools, showers, or gyms can help avoid coming into contact with the fungus.
Health of the immune system: Overall health, including the management of underlying conditions like diabetes or immune disorders, can reduce the risk of fungal infection.
Conclusion:
Proximal subungual onychomycosis is a fungal nail infection that starts at the base (proximal) of the nail and may lead to discoloration, thickening, and deformation of the nail. It is most commonly caused by dermatophytes or Candida, especially in people with weakened immune systems or nail trauma. Diagnosis results from clinical examination and laboratory findings, and the treatment may comprise local or systemic antifungals, plus nail debridement in specific cases. Maintaining the prevention of moisture trapping and protection of the nails against injury should minimize the risk of acquiring this disorder.
Would you like information regarding treatment or prevention?
Endonyx onychomycosis is a rare form of nail fungus (onychomycosis) in which the fungal infection involves the inner layers of the nail plate rather than the surface. In contrast to other forms of onychomycosis, which usually involve the outer or superficial layers of the nail, endonyx onychomycosis involves deeper penetration within the nail structure itself. Endonyx onychomycosis may result in thickening, discoloration, and deformation of the nail.
Key Features of Endonyx Onychomycosis:
Appearance:
The nails are typically discolored—typically white, yellow, or brown.
The nail plate may become thick and opaque as the infection is in the deeper structures of the nail.
The infection doesn’t usually affect the surface of the nail but can cause big alterations to the shape of the nail.
In some cases, the infected nail may become twisted or distorted as the infection progresses.
Subungual hyperkeratosis (tissue thickening beneath the nail) is frequent and tender.
Causes:
Endonyx onychomycosis is caused primarily by dermatophytes, specifically Trichophyton species (e.g., Trichophyton rubrum, Trichophyton mentagrophytes).
Fungus infests the nail bed and progresses inwardly, infecting the inner portions of the nail plate. The infection will not typically progress to the nail’s surface or surrounding skin because it is confined to the nail matrix and internal tissue.
Like other types of onychomycosis, wet environments, poor individual cleanliness, and nail trauma are accountable for creating the infection.
Risk Factors:
Trauma or injury to the nail, which may allow fungi to invade deeper tissues.
Recurrent exposure to moisture, such as in swimming or wearing tight shoes.
Diabetes, immunocompromised states, and other systemic illnesses that predispose to infection.
Poor or improper nail care, which can lead to predisposition to fungal infection.
Symptoms:
The nails may become opaque and discolored, yellowish, white, or brownish in color.
The infection is usually confined to the nail plate, but with time, the nail gets thickened and deformed.
Unlike other forms of onychomycosis, endonyx onychomycosis cannot always lead to obvious nail lifting and separation from the nail bed (onycholysis) in the early stages.
The infected nail may be rough, brittle, and fragile.
Diagnosis:
Clinical Exam: A physician will inspect the nail for any sign of discoloration, thickening, or structural change typical of endonyx onychomycosis.
Microscopic Exam or Culture: Nail scrapings are collected and examined microscopically or cultured for fungus to confirm the diagnosis and isolate the causative fungal pathogen.
Dermatophyte Detection: The causative dermatophyte species is determined by fungal cultures or PCR reactions.
Treatment
Treatment of Endonyx onychomycosis may be challenging, and it could be a combination of the following:
Topical Antifungals:
Amorolfine nail lacquer or ciclopirox lacquer can be applied to the affected nails, but these are more useful in mild to moderate infection and could take months to act.
Topical antifungals must often be used long-term to clear the fungus out of deeper structures of the nail.
Oral Antifungal Medications:
Terbinafine, itraconazole, and fluconazole are the most frequently used oral antifungals in the treatment of onychomycosis, including endonyx onychomycosis.
Topical therapy is usually reserved for less severe cases that are resistant to topical therapy.
The drug can need to be taken for a period of weeks to months, depending on the extent of severity and growth rate of the nails.
Nail Debridement:
On certain occasions, debridement of the nail by removing or cutting the infected nail may reduce the fungal load and enhance the effectiveness of antifungal treatment.
This is done manually or with laser therapies that kill the fungal infection without damaging the nail.
Laser Therapy:
Laser treatment, either Nd:YAG laser or laser light therapy, has been found helpful in the treatment of onychomycosis fungal infections such as endonyx onychomycosis. The treatment kills and destroys the fungus cells in the nail using light or heat.
Prognosis:
Prognosis of endonyx onychomycosis is good but may be found challenging to cure as a chronic infection. The nail can return to a normal position with proper antifungal therapy.
Total treatment and eradication of the fungus can take a few months due to the gradual growth of nails.
Prevention:
Nail hygiene: Cleaning, drying, and cutting the nails can avoid fungal infections.
Evading nail trauma: Evading damage or trauma to the nails reduces the risk of fungi entering the nail bed.
Shoes: Wearing shoes that allow for air circulation of the feet and avoid excessive moisture can avoid fungal growth.
Early treatment of athlete’s foot or other fungal infections of the nails can prevent spreading to the nails.
If you would like more information about treatment choices or specific management of endonyx onychomycosis, simply ask!
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!