Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is distal subungual onychomycosis?
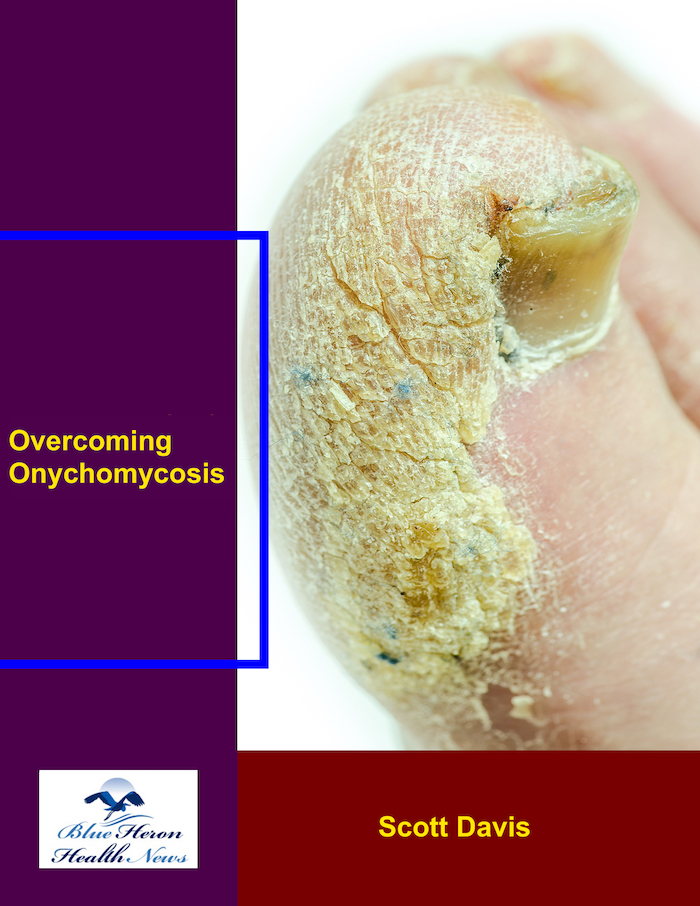
Distal subungual onychomycosis (DSO) is the most common type of nail fungus (onychomycosis) and affects the toenails or fingernails, specifically the distal (terminal) end of the nail and the nailbed below. It is caused by dermatophytes, a skin, hair, and nail-infecting fungus.
Key Features of Distal Subungual Onychomycosis:
Location:
The infection typically begins at the distal edge of the nail (the most distant point from the nailbed) and works its way inward toward the nailbed.
The fungus grows between the nail plate and the nailbed, causing thickening, discoloration, and brittleness of the nail.
Appearance:
Thickened nails: The infected nail may thicken and be hard to cut.
Discoloration: The nail typically turns yellowish, white, or brown due to the buildup of fungal infection under the nail.
Debris under the nail: White or yellowish debris is found under the nail plate.
Crumbly edges: The edges of the nail become crumbly or rough as the infection progresses.
Separation: In severe cases, the nail can lift or separate from the nailbed (onycholysis).
Symptoms:
Nail sensitivity or pain: The infected nail is painful and hurts when there is pressure put on the nail.
Foul odor: In other cases, there is the emission of a foul odor from the infected nail due to the fungal infection.
Distortion of the nail: The nail deforms or loses its normal shape as the infection progresses.
Dermatophytes, fungi that thrive in warm and moist environments, are responsible for the infection. The two most common dermatophyte species that infect and lead to DSO are Trichophyton rubrum and Trichophyton mentagrophytes.
The infection may occur when the nail is exposed to moist environments, like wearing tight shoes, sweating, or walking barefoot in public places like swimming pools or shower stalls.
Nail damage also makes one susceptible to fungal infection since it offers a channel through which the fungus will enter the nailbed.
Risk Factors:
Advanced age: The condition is more common among older individuals, whose nail growth slows down and whose immune system weakens with age.
Diabetes: Diabetic patients are also more likely to be infected by fungi, especially of the foot.
Poor circulation: Illnesses that damage blood flow, such as peripheral artery disease, can cause the body to have a harder time fighting off infection.
Immunocompromised patients: Patients with weakened immune systems (e.g., due to HIV, chemotherapy, or some medications) are more susceptible to DSO infection.
Fungal infections elsewhere on the body: History of fungal infections of the skin or other nails puts them at risk for nail infection.
Diagnosis:
Clinical examination: The diagnosis is typically established by a medical practitioner on the basis of the appearance of the nail.
Laboratory tests: A sample from the infected nail may be taken to identify the causative fungus. This may be done through microscopic examination, culture, or PCR.
Treatment:
Topical antifungal drugs: Creams, ointments, or lacquers (like ciclopirox nail lacquer) can be used, but maybe not so well for more serious infections.
Oral antifungal medications: For more extensive or serious infections, oral medications like terbinafine, itraconazole, or fluconazole are administered. These medications target the fungi internally.
Nail debridement: On a few occasions, the diseased nail piece has to be cut or avulsed for the antifungal medicine to penetrate more easily.
Laser therapy: On a few occasions, laser treatment can be used to kill nail fungal infections by destroying the cells of the fungi.
Prevention:
Good foot hygiene: Having dry, clean feet and wearing socks frequently may be used for preventing fungus from growing.
Avoiding shared wet facilities: Being barefoot or using water shoes or sandals at public showers, pools, and gyms can reduce exposure to the fungus.
Proper footwear: Wearing ventilated footwear and socks that wick away moisture from the feet can hinder fungal infection.
Preventing infection of the nails: Protecting the nails from injury can block channels for the fungus.
Distal subungual onychomycosis is a common fungal nail infection that is characterized by thickening, discoloration, and potential separation of the nail from the nailbed. It is caused by dermatophyte fungi, typically in patients who have risk factors such as older age, diabetes, or circulatory issues. Early diagnosis and effective treatment, including antifungal medication, can cure and manage the infection. Prevention of recurrence can be done through proper care of the nails and hygiene practices.
Would you rather hear more information on treatment or prevention strategies for this condition?
White superficial onychomycosis (WSO) is a fungal nail disease that affects primarily the distal portion of the nail plate, causing patches or spots of whitish color change. White superficial onychomycosis is one of many types of onychomycosis (fungal infections of the nail), which may occur on either the toenail or fingernail, but it is seen more frequently on the toenail.
Key Features of White Superficial Onychomycosis:
Appearance:
White, powdery or chalky streaks or patches on the nail surface.
With progression of the disease, the nail plate becomes crumbly or rough, and the patches of white spread over the nail.
The infection is typically superficial and does not extend to the deeper structures of the nail or other tissues.
Causes
White superficial onychomycosis is most commonly caused by dermatophytes (fungi that infect skin, hair, and nails), specifically the pathogens Trichophyton mentagrophytes and Trichophyton rubrum.
The infection typically occurs when fungus spores are exposed to a nail surface and have a suitable environment in which to grow, such as warm, moist conditions.
Risk Factors:
Poor nail hygiene or nail damage that creates an opening for fungi.
Overhydration, especially in environments like public pools or locker rooms.
Diabetes, immunocompromised states, and other chronic health conditions that compromise immune response.
Wearing closed, tight shoes that cause heat and moisture buildup.
Fungal infections of the skin like athlete’s foot that can spread to the nail.
Symptoms:
White streaks or patches that are observable on the surface of the nail.
Thickening, crumbling, or color alteration of the infected nail.
In worse cases, the nail may grow brittle and start to peel off from the nail bed.
Diagnosis:
Visual examination: WSO can be diagnosed by a doctor based on its whiteness and superficial position.
Microscopic examination or culture: In order to confirm the diagnosis and rule out other types of nail infection, a sample of the nail scraping might be examined microscopically or cultured to identify the pathogenic fungus.
Treatment:
Topical antifungals: White superficial onychomycosis is commonly managed with the first-line choice of applying antifungal ointments, creams, or lacquers to the infected nails. Ciclopirox and amorolfine are two such antifungal lacquers.
Oral antifungals: In the event of widespread infection or non-response to topical agents, oral antifungals terbinafine or itraconazole may be employed.
Nail debridement: Regular filing and trimming of the infected nails can be useful to remove infected tissue and make topical treatments more effective.
Good nail hygiene: Trimming, drying, and cleaning nails helps prevent infection from spreading and heals the area.
With proper treatment, white superficial onychomycosis can be usually cured and the infected nail should then grow out normally. Treatment will most likely take weeks to months, depending on how severe the infection is and how fast the nail grows.
Would you like more information about treatment options or the prevention of onychomycosis in general?
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!