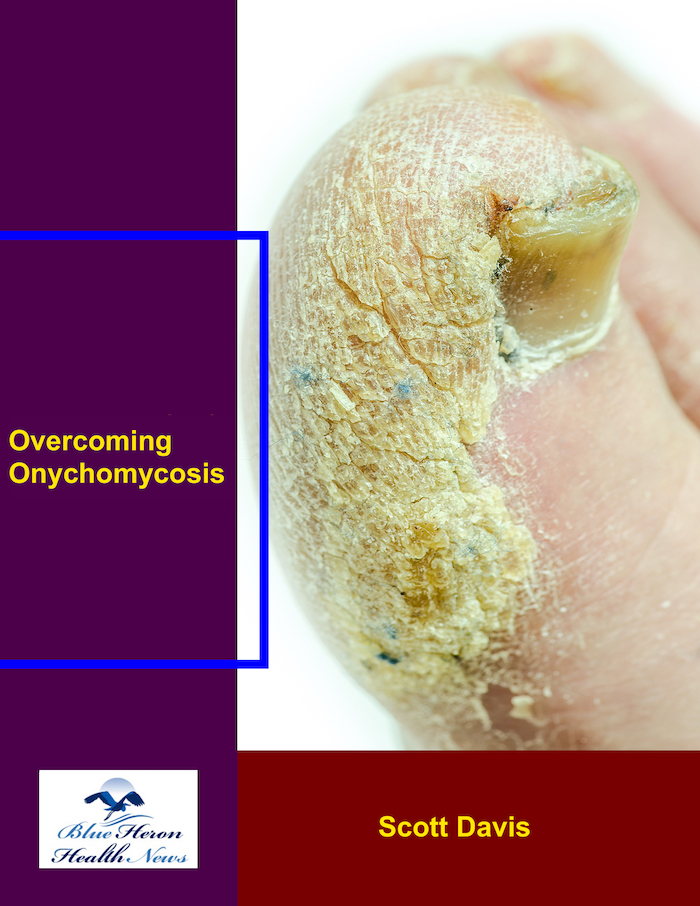
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What are the challenges of diagnosing onychomycosis in elderly patients?
Diagnosis of onychomycosis in the elderly patient may be particularly challenging due to several factors, including overlapping with other aging conditions, compromised immune function, and other coexisting medical conditions. These factors may cause delay in diagnosis and also complicate treatment. The following is a detailed analysis of the specific challenges:
1. Overlap with Other Nail Conditions
Age-Related Nail Changes: With increasing age, the growth of the nails slows down, and the nails become thickened, colored, and prone to brittleness. Such physiological age-related changes can resemble onychomycosis, and therefore, it is often difficult to distinguish between onychomycosis and other common age-related changes in nails.
Psoriasis or Eczema: Psoriasis, a disease of the aged, may result in pitting, thickening, and discoloration of nails, similar to those of onychomycosis. Similarity in presentation makes diagnosis a challenge because these may be wrongly diagnosed as non-fungal infection by clinicians.
Trauma: The elderly person may be affected by nail trauma due to accidents or common wear and tear of the nail plate, and its discoloration or deformation will be misleading, simulating the fungal infection.
2. Subtle Onset and Slow Progression
Slow Onset: In elderly patients, onychomycosis may be slower in onset and more subtle in presentation, with a minor thickening or pigmentation that may not be immediately noticeable. The slow onset leads to delayed diagnosis, with the symptoms being misinterpreted as aging or disregarded.
Mild Symptoms: Older patients may not even feel the pain or itching experienced by younger individuals, and the infection may not be noticed and thus delay treatment.
3. Decreased Immune Function
Weakened Immune System: Aging is often associated with reduced immune function (immunosenescence) that predisposes older individuals to become more susceptible to infection, including fungal infection. But the compromised ability of the immune system to respond to fungal pathogens can result in less dramatic symptoms, presenting a diagnostic challenge.
Chronic Conditions: Older patients are likely to have chronic diseases (e.g., diabetes, cardiovascular disease, or autoimmune diseases) that affect the immune system and might contribute to fungal infection risk. However, such underlying diseases can mask or alter the classic presentation of onychomycosis.
4. Concurrent health conditions
Diabetes and Vascular Disease: Elderly patients frequently have vascular disease or diabetes that can cause circulatory impairment, especially of the feet. This makes infection harder to notice because the poor circulation may block normal symptoms (e.g., redness, swelling) from appearing.
Peripheral Neuropathy: Peripheral neuropathy, which is common among the elderly, may lead to numbness or loss of sensation in the feet, and also make it harder for patients to feel early signs of nail infection.
Multiple Medications: Elderly patients are often administered multiple medications that can interact with antifungal treatment or mask signs of infection. For example, immunosuppressive drugs can weaken the body’s ability to fight off fungal infection, thereby making diagnosis more challenging.
5. Difficulty in Diagnostic Testing
Nail Sampling and Sensitivity: It is more difficult to take a nail scraping or specimen for fungal culture in the elderly due to thickened or brittle nails, especially in those with widespread onychomycosis. This can result in false-negative results if a poor sample is taken.
Delayed Diagnosis on the Basis of Test Procedure: Optimal diagnosis most often translates into referral of samples for fungal cultures or microscopy, both of which are slow. In the elderly patient, this delay in diagnosis can result in progression of the infection before appropriate treatment is begun.
6. Cognitive Impairment
Memory Issues: Dementia or cognitive impairment is common among elderly populations and may affect the patient’s ability to notice symptoms like pain or color changes in their nails. This will lead to delayed medical treatment, and thus the infection will remain untreated for a longer duration.
Lack of Awareness: Older adults may not be aware or may disregard minor differences in the color and texture of their nails, especially if they are preoccupied with more serious health problems. Cognitive impairment can also prevent them from feeling the need for treatment.
7. Misdiagnosis or Underdiagnosis
Attribution to Age: Because onychomycosis is more common in older individuals, color or texture alterations in the nails due to onychomycosis can be inappropriately attributed to the aging process. Clinicians might thus overlook the diagnosis of fungal infection and attribute nail color or texture changes to normal aging and not to an amenable condition.
Underrecognition by Healthcare Providers: Because onychomycosis is challenging to diagnose in elderly patients, healthcare providers might not rank it as a priority diagnosis, especially when symptoms are minimal or accompanied by other age-related conditions.
8. Reduced Treatment Compliance
Treatment Complexity: Treatment of onychomycosis in the elderly can be complicated by the need for prolonged treatment (e.g., weeks or months of oral antifungals) or taking topical therapy that requires frequent application. Elderly patients may have trouble following through with the selected treatment regimen, especially if they have more than one disease to treat.
Potential Drug Interactions: Older patients are usually on medication for other chronic conditions. The possibility of drug interaction with oral antifungal therapy (e.g., liver damage with itraconazole or terbinafine) can limit the selection of therapy or require close follow-up, making treatment more complicated.
9. Impact of Nail Deformities and Aesthetic Concerns
Decreased Concern about Cosmetic Issues: Cosmetic issues about the appearance of the nails may be of lesser significance in older patients. This might lead to failure to report the symptoms or to present for treatment when the infection has already progressed significantly.
Psychosocial Impact: Aesthetic impact in onychomycosis, for instance, discoloration or distortion of the nail, could cause embarrassment or reduce the quality of life among certain older individuals. Since they may not treat the infection due to the fungus as an emergency as for other acute conditions, it becomes unmanaged.
Conclusion
Diagnosis of onychomycosis in the older patient poses unique challenges, from overlap of symptoms with common aging changes of the nails to the presence of multiple conditions that may mask or obscure diagnosis. In addition, compromised immune status, dementia, and difficulty with diagnostic testing can all lead to delays in infection diagnosis and treatment. Healthcare providers should pay attention to these challenges and add onychomycosis to their differential diagnosis, even in the presence of other frequent age-related changes, to offer timely treatment and prevent possible complications.
Duration of infection can affect onychomycosis diagnosis greatly in different ways. While duration of infection itself does not alter the diagnostic tests utilized, it can exert an effect on how the disease will present, on how difficult the diagnosis would be, and on how clinicians manage the disease. The following is how onychomycosis duration affects the diagnostic process:
1. Clinical Presentation
Chronicity and Severity
Increased Duration: More chronic or longer-standing infections are more severe and may have more significant nail changes such as hyperthickening, discoloration, deformities, and extensive onycholysis. These changes also increase the likelihood of the infection being diagnosed based on visible clinical findings.
Shorter Course: Acute or initial onychomycosis may be present with less obvious signs such as slight discoloration or local thickening of the nail. In these cases, the infection may be less obvious, and it becomes harder to diagnose by external appearance, especially if the patient or child does not present with more obvious signs.
2. Problems in Diagnosing Chronic Infections
Features Contributing Complexity to Chronic Infections
Superimposed Bacterial Infection: Secondary bacterial infection may complicate long-standing or chronic onychomycosis. It may cause additional nail modifications, including enhanced redness, heat, or purulent drainage, that otherwise might suggest a bacterial infection rather than a fungal etiology. The clinician needs to differentiate between the fungal infection and secondary bacterial infections.
Nail Deformities: Chronic infection may cause severe nail damage, and it might be more challenging to distinguish fungal infection from other etiologies (e.g., trauma, psoriasis). Nails may become deformed or thickened with time, and the fungal infection may no longer be readily identified on the standard clinical examination, and additional tests like microscopic examination or fungal culture would be necessary to identify the etiology.
3. Long-Term Fungal Growth
Fungal Load: Increased fungal load may be present in chronic infections. Increased fungal load means that greater numbers of fungal structures (e.g., spores or hyphae) are likely to be found in nail clippings or in scrapings and thus are more likely to be detectable by culture or microscopic examination. This could allow clinicians to make a diagnosis later on.
4. Diagnostic Timeframe and Treatment Response
Confirmation of Diagnosis: The longer the duration of the infection, the higher the chances of nail change advancing to a position where it becomes unequivocally diagnostic of onychomycosis. With new infections, nail changes tend to be subtle and could be confused with other conditions, for example, eczema or psoriasis. In such cases, diagnostic processes such as microscopic examination, culture for fungi, or polymerase chain reaction (PCR) would need to be undertaken to determine diagnosis.
Treatment Monitoring: Duration of infection also decides on which basis treatment response is followed up. In chronic infections, a longer course of treatment or combination of both topical and systemic antifungals is done depending on the degree of the infection and nature of the fungus. The clinician may also need to monitor for recurring infections, especially in instances of chronic infection or when the patient has an underlying risk factor, such as diabetes or compromised immunity.
5. Regrowth of Nail and Diagnosis
Impact on Nail Growth: Chronic onychomycosis can lead to permanent destruction of the nail, with the nail not regrowing normally despite successful eradication of the fungus. If infection has been of long duration, regeneration of the nail is late and may never fully return to its preexisting state, especially in infections which have resulted in severe damage to the nail matrix.
Assessment of Treatment Success: In chronic-duration infections, regrowth of the nail is often used as a significant marker for the assessment of treatment success. A normally appearing nail after treatment suggests that the infection was well treated, while repeated nail abnormalities can suggest either treatment failure or re-infection.
6. Distinguishing from Other Chronic Diseases
Chronic Conditions Suggestive of Onychomycosis: In addition to chronic conditions that have existed for many years or several months, other chronic diseases of the nail such as eczema or psoriasis may also produce nail changes virtually indistinguishable from those seen in onychomycosis. The chronic nature of the disease will then obscure the diagnosis in such cases because the presentation will overlap. Therefore, proper patient history, clinical examination, and laboratory investigation is necessary to exclude other causes of fungal infection.
Conclusion
The chronic nature of onychomycosis largely determines the mode of diagnosis of the infection. More chronic cases are more likely to present with more severe and noticeable symptoms facilitating diagnosis but potentially complicating the clinical presentation due to potential secondary bacterial infection or nail deformation. Also, in chronic infections there may be increased fungal loads that are easier to diagnose the causative organism, but they may require longer treatment or more intense follow-up. Conversely, in acute infections symptoms may be less severe and be harder to diagnose by observation alone, requiring further lab work for a definitive diagnosis.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!