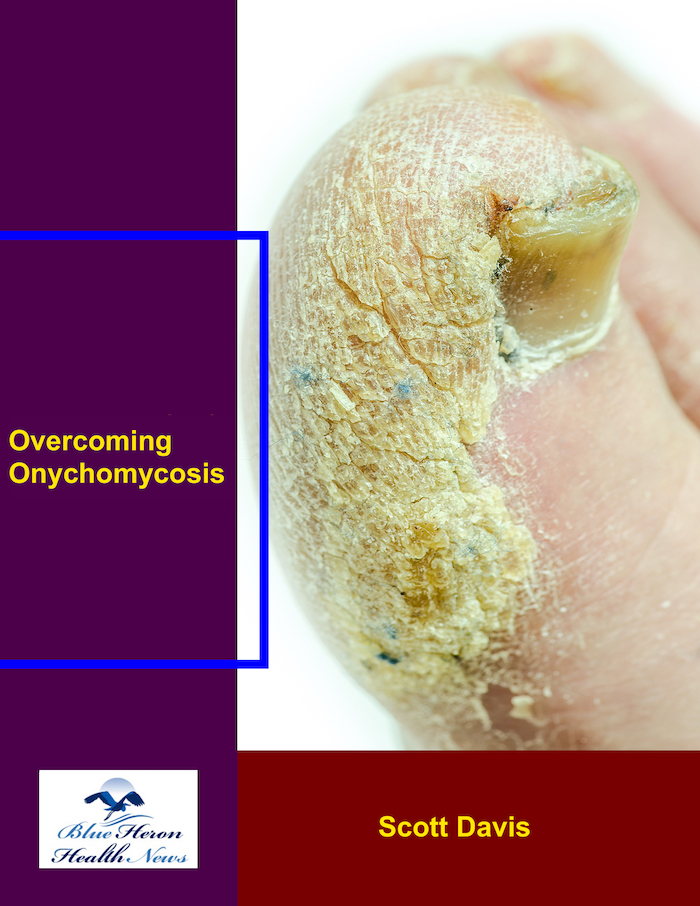
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is the role of clinical history in diagnosing onychomycosis?
The Role of Clinical History in Diagnosing Onychomycosis
A detailed clinical history is crucial in diagnosing onychomycosis because fungal nail infections can mimic other nail conditions. Understanding a patient’s risk factors, symptoms, and medical background helps differentiate onychomycosis from non-fungal nail disorders and guides the decision for laboratory testing.
1. Identifying Risk Factors for Onychomycosis
Certain factors increase the likelihood of developing onychomycosis. A clinical history helps determine if a patient is at higher risk.
A. Personal Risk Factors
- Age: More common in older adults due to slower nail growth and reduced immune response.
- Diabetes: Increases susceptibility to fungal infections due to poor circulation and immune dysfunction.
- Peripheral Vascular Disease: Reduced blood flow can make nails more prone to infection.
- Immunosuppression: Conditions like HIV/AIDS or medications like steroids and chemotherapy weaken the immune system, increasing fungal infection risk.
B. Lifestyle and Environmental Factors
- Frequent Exposure to Moisture: Wearing damp socks, sweaty shoes, or walking barefoot in public areas (pools, gyms) raises the risk.
- Nail Trauma: Repetitive injury or pressure (e.g., from tight shoes) can create entry points for fungal infection.
- Poor Foot Hygiene: Lack of proper nail care, such as trimming nails improperly, can increase susceptibility.
C. Family and Medical History
- Family history of fungal infections: Some individuals may have a genetic predisposition to onychomycosis.
- Previous fungal infections: A history of athlete’s foot (tinea pedis), jock itch, or skin fungal infections can increase the likelihood of nail involvement.
- Concurrent skin conditions: Psoriasis, eczema, and lichen planus can cause nail changes similar to onychomycosis.
2. Assessing Symptoms and Nail Changes
A clinical history helps determine how the nail changes developed over time.
Key Questions to Ask
- When did the nail changes start?
- Onychomycosis is slowly progressive, whereas trauma or bacterial infections often appear suddenly.
- Are the nails painful or just discolored?
- Fungal infections usually don’t cause pain unless severe.
- Are there associated symptoms like itching or foot scaling?
- Presence of itchy, scaly skin suggests a coexisting fungal skin infection (e.g., athlete’s foot).
- Do multiple nails or just one nail show changes?
- Onychomycosis usually spreads gradually to multiple nails, while trauma typically affects one nail.
- Have you used any prior treatments?
- Some patients may have self-treated with over-the-counter antifungals, which could affect test results.
3. Differentiating Onychomycosis from Other Nail Conditions
A thorough clinical history helps rule out non-fungal nail disorders, which require different treatments.
| Condition | How Clinical History Helps in Differentiation |
|---|---|
| Onychomycosis | Gradual nail thickening, discoloration (yellow/white), no pain unless severe. History of fungal infections or risk factors. |
| Psoriasis | History of skin psoriasis or joint pain. Nails show pitting, oil-drop discoloration, and ridging (not seen in fungal infections). |
| Trauma | History of nail injury, rapid color change (black, red, or blue), no fungal exposure. |
| Lichen Planus | History of itchy, purple skin lesions, nail ridging, and thinning. Usually affects multiple nails symmetrically. |
| Bacterial Paronychia | Sudden swelling, pain, and pus around the nail. Often linked to nail biting or excessive moisture exposure. |
4. Guiding Laboratory Testing
After taking a clinical history, doctors decide whether to proceed with:
- Microscopic examination (KOH test) to detect fungal hyphae.
- Fungal culture to identify the specific fungus.
- Nail biopsy if the diagnosis is unclear.
Conclusion
A thorough clinical history helps identify risk factors, assess symptoms, differentiate from other conditions, and guide testing. Since onychomycosis can resemble other nail disorders, accurate history-taking is essential for proper diagnosis and treatment.
Would you like to explore treatment options or ways to prevent onychomycosis recurrence?
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!