Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
How is onychomycosis diagnosed?
Onychomycosis (fungal nail infection) is diagnosed through a combination of clinical examination, laboratory tests, and sometimes imaging. Here’s how the diagnosis is typically made:
1. Clinical Examination
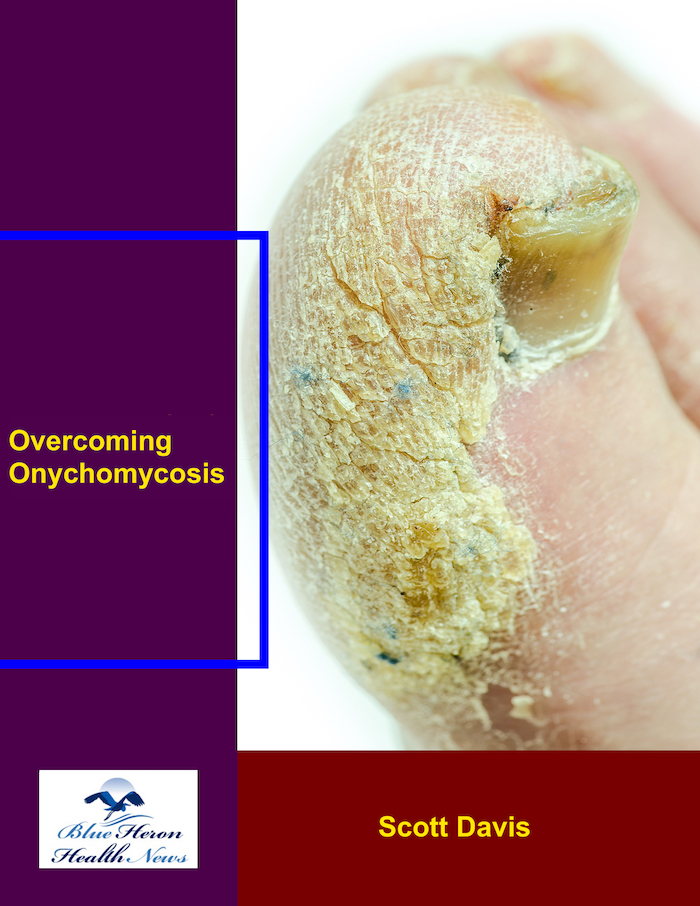
The first step in diagnosing onychomycosis involves a thorough physical examination of the affected nails. Common signs of onychomycosis include:
- Thickened nails: The nails may appear thick and distorted.
- Discoloration: The nails may appear yellow, white, or brown.
- Brittleness or crumbling: The infected nails may become brittle, crumble, or break easily.
- Debris under the nail: There may be white or yellowish debris under the nail.
- Separation of the nail from the nail bed (onycholysis): The nail may lift away from the skin beneath it.
The doctor will also inquire about any risk factors, such as trauma, diabetes, poor foot hygiene, or immunocompromised states, which can increase the risk of fungal nail infections.
2. Laboratory Tests
Since other conditions can mimic the symptoms of onychomycosis (such as psoriasis or trauma), laboratory tests are necessary to confirm the diagnosis and identify the specific fungal organism causing the infection.
Common tests include:
- KOH (potassium hydroxide) preparation: A sample of nail debris is scraped from the affected nail and treated with a solution of potassium hydroxide. If fungal elements (such as hyphae or spores) are present, they will be visible under a microscope, confirming the fungal infection.
- Fungal culture: A small sample of nail tissue or debris is collected and sent to a laboratory where it is cultured to allow fungi to grow. This test helps identify the specific type of fungus causing the infection (e.g., dermatophytes, yeasts, or non-dermatophyte molds). Fungal culture is a more sensitive test than KOH but may take longer (usually 2-4 weeks).
- PCR (Polymerase Chain Reaction): This molecular test detects the genetic material of fungi in the nail sample. It is more sensitive than a culture and can identify the specific fungal species involved, although it is typically used in specialized labs.
3. Histopathology
- In some cases, a nail biopsy may be performed if the diagnosis is unclear or if there is suspicion of other conditions. This involves taking a small piece of the affected nail or nail bed tissue for microscopic examination. Histopathology can provide more detailed information about the infection and rule out other potential causes.
4. Wood’s Lamp Examination
- A Wood’s lamp (a UV light) can sometimes be used to assess fungal infections. When fungi like Microsporum species are present, they will fluoresce under UV light. However, this is not commonly used for diagnosing onychomycosis, as it is more effective in diagnosing fungal infections of the skin, such as ringworm.
5. Differentiation from Other Conditions
Onychomycosis symptoms can overlap with other nail conditions, such as:
- Psoriasis: Psoriasis can cause nail changes, including pitting, discoloration, and thickening. A detailed medical history and clinical examination help differentiate between fungal infections and psoriasis.
- Trauma or injury: Trauma to the nail can cause discoloration, thickening, or separation of the nail from the nail bed. This can sometimes be mistaken for a fungal infection, but the history of an injury or trauma will help distinguish the two.
- Bacterial infections: Some bacterial infections can cause swelling, redness, and pus under the nail, resembling fungal infections. These are differentiated through culture tests, which will identify bacteria rather than fungi.
6. Imaging (Rare)
- In rare cases, X-rays or nail ultrasound might be used if there is suspicion of significant bone involvement or if the infection has progressed to a severe stage, but this is not routine for diagnosing onychomycosis.
Summary of Diagnostic Methods:
- Clinical Examination: Observing the appearance of the nails.
- KOH Preparation: Scraping and examining under a microscope for fungal elements.
- Fungal Culture: Growing the fungus to identify the type of organism.
- PCR Testing: Detecting fungal DNA for more precise identification.
- Histopathology: Examining tissue samples for fungal infection.
- Wood’s Lamp: UV light to detect certain fungal species (less common).
- X-rays or Ultrasound: In rare cases, to check for bone or deeper tissue involvement.
Conclusion:
The diagnosis of onychomycosis involves a combination of clinical evaluation, laboratory testing, and sometimes imaging or biopsy. Identifying the specific fungal pathogen through tests like fungal culture or PCR helps determine the appropriate treatment. Early diagnosis and proper identification of the pathogen are important for effective treatment and to prevent recurrence.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!