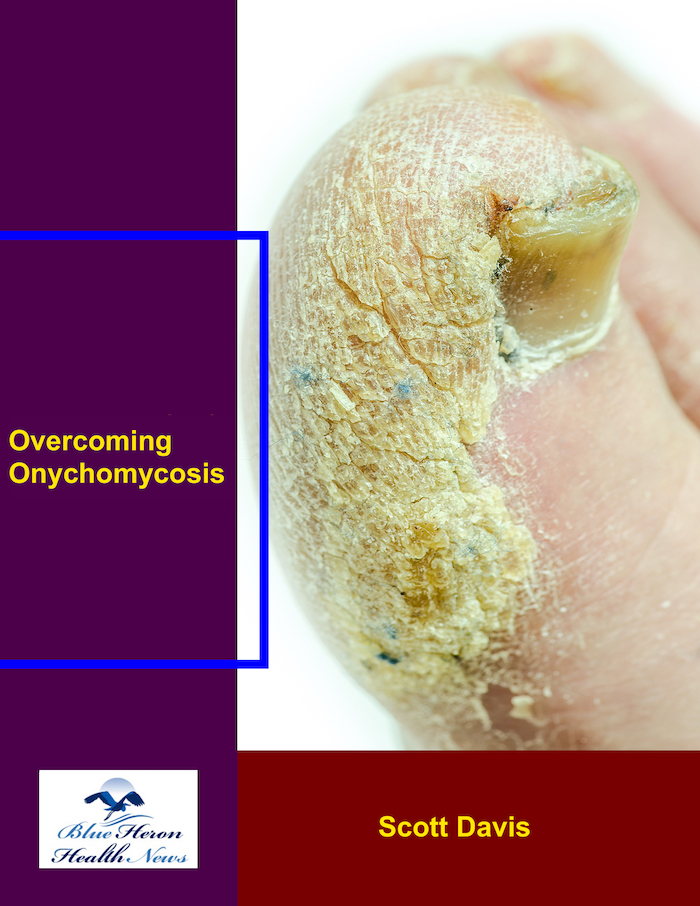
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is the role of yeast in causing onychomycosis?
Yeasts, particularly species of the genus Candida, play a notable role in causing certain types of onychomycosis, although dermatophytes (fungi that infect keratinized tissues) are the more common cause. When yeasts are involved, they typically cause a subtype of onychomycosis called candidal onychomycosis. Here’s how yeast contributes to onychomycosis:
1. Common Yeast Species:
- The most common yeast involved in onychomycosis is Candida albicans, but other species like Candida parapsilosis and Candida tropicalis can also cause infection.
- Candida species are opportunistic pathogens, meaning they normally live harmlessly on the skin and mucous membranes but can cause infection under certain conditions, particularly when the immune system is compromised or the nail environment becomes favorable for fungal growth.
2. Mechanism of Infection:
- Candidal onychomycosis usually occurs when there is damage to the nail, such as from trauma, frequent immersion in water, or preexisting nail disease.
- Yeasts can invade the nail bed and nail plate, causing infection that often begins in the proximal (closer to the cuticle) or lateral (sides of the nail) regions, unlike dermatophyte onychomycosis, which usually starts at the distal (tip) edge of the nail.
3. Predisposing Factors:
Several conditions increase the likelihood of yeast-causing onychomycosis:
- Immune system compromise: People with weakened immune systems (e.g., due to diabetes, HIV, or immunosuppressive therapies) are more susceptible to Candida infections, including those of the nails.
- Moist environments: Candida thrives in warm, moist environments. Individuals with occupations or habits that involve frequent wetting of the hands (such as dishwashers, cleaners, or healthcare workers) are at higher risk.
- Paronychia (inflammation of the skin around the nail): Chronic paronychia, especially in people who have wet hands frequently, is often associated with Candida. The infection can spread from the surrounding skin to the nail itself, leading to candidal onychomycosis.
- Nail trauma or damage: Trauma to the nail or nail bed, especially repetitive trauma or pressure, can create openings for Candida to invade.
4. Symptoms of Candidal Onychomycosis:
- The infected nail may become thickened, discolored (yellow, white, or brown), and brittle, similar to dermatophyte-related onychomycosis.
- Unlike dermatophyte infections, swelling, redness, and inflammation around the nail (paronychia) are more common in candidal infections.
- In severe cases, the nail may separate from the nail bed (onycholysis), and the nail plate may be damaged or destroyed.
5. Difference from Dermatophyte Onychomycosis:
- Location of infection: Candidal onychomycosis often starts near the cuticle (proximal part) or side of the nail, whereas dermatophyte infections usually begin at the distal edge of the nail.
- Associated conditions: Candidal infections are more commonly associated with chronic skin inflammation, wet environments, and conditions that compromise the immune system.
- Faster progression: Candidal onychomycosis tends to progress more rapidly than dermatophyte infections.
6. Treatment of Candidal Onychomycosis:
- Topical antifungals: Medications like ciclopirox and amorolfine may be prescribed, but they are generally less effective for yeast infections than systemic treatments.
- Oral antifungals: Oral treatments like itraconazole or fluconazole are often more effective for candidal onychomycosis, especially in cases of extensive infection or involvement of multiple nails.
- Managing underlying conditions: It’s important to address factors that contribute to candidal growth, such as moisture, trauma, or other infections. In people with chronic paronychia, managing the inflammation around the nail is crucial to prevent recurrence.
- Prevention: Keeping nails dry, avoiding excessive water exposure, and maintaining good hand and nail hygiene are important steps in preventing candidal infections.
7. Role in Mixed Infections:
- Yeasts can sometimes be part of mixed infections in the nail, where both dermatophytes and yeasts are present. This complicates diagnosis and treatment since both types of fungi may need to be addressed with a combination of antifungal therapies.
Summary:
While yeasts like Candida are less common causes of onychomycosis compared to dermatophytes, they are significant in certain populations and under specific conditions, particularly where moisture, trauma, or immune system issues are present. Candidal onychomycosis tends to involve the proximal nail and is associated with inflammation around the nail. Treatment involves both topical and systemic antifungal medications, along with addressing the environmental factors that favor yeast growth.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!