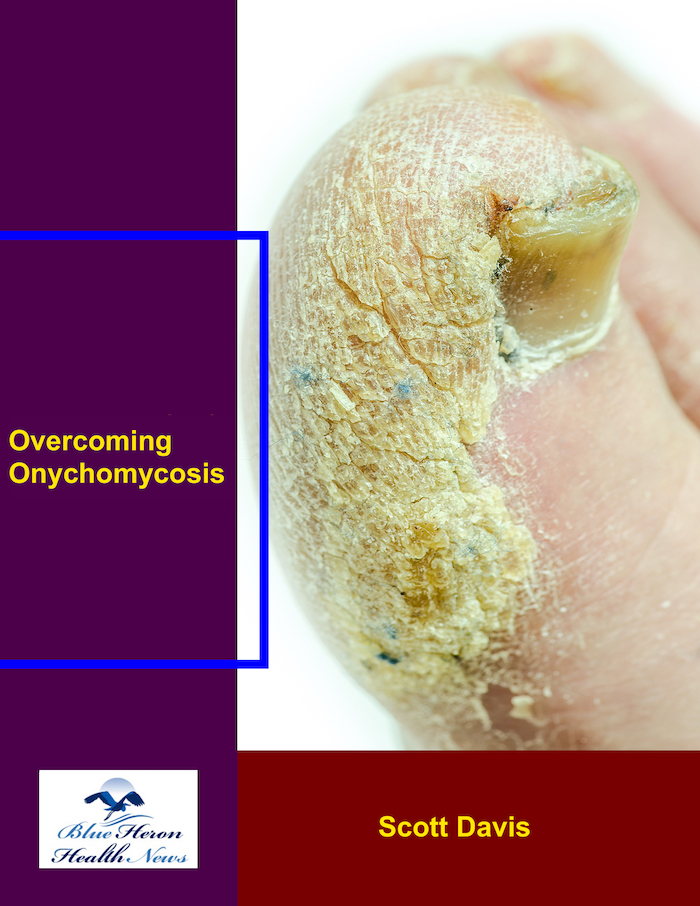
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
What is white superficial onychomycosis?
White superficial onychomycosis (WSO) is a type of fungal nail infection characterized by white, chalky patches or spots on the surface of the nail plate. Unlike other forms of onychomycosis that primarily affect the nail bed, WSO affects the top layers of the nail. This type of infection is relatively uncommon compared to distal subungual onychomycosis but can still lead to significant nail changes.
Key Characteristics and Symptoms
- White Spots or Patches:
- The most distinctive feature of WSO is the presence of white, opaque patches or spots on the surface of the nail. These can vary in size and may spread across the entire nail surface if left untreated.
- Chalky Appearance:
- The affected areas of the nail often have a chalky or powdery appearance. The nail surface may become rough and crumbly as the infection progresses.
- Superficial Infection:
- The fungal infection in WSO remains superficial, affecting only the outermost layers of the nail plate. This differentiates it from other types of onychomycosis, where the infection can penetrate deeper into the nail bed and matrix.
- Minimal Nail Thickening:
- Unlike other forms of onychomycosis, WSO typically does not cause significant thickening of the nail. The main changes are in the color and texture of the nail surface.
Causes
White superficial onychomycosis is most commonly caused by dermatophyte fungi, particularly Trichophyton mentagrophytes. However, non-dermatophyte molds and yeasts can also cause WSO, especially in immunocompromised individuals. The fungi invade the superficial layers of the nail, breaking down keratin and leading to the characteristic white patches.
Risk Factors
- Moist Environments: Like other fungal infections, WSO is more likely to develop in conditions where the nails are frequently exposed to moisture, such as in communal showers or swimming pools.
- Nail Trauma: Damage to the nail can increase the risk of infection by providing an entry point for fungi.
- Immunocompromised State: Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk for developing WSO and other fungal infections.
Diagnosis and Treatment
Diagnosis of WSO involves a physical examination of the affected nails and laboratory tests, such as KOH preparation, fungal culture, or PCR testing, to identify the causative organism.
Treatment Options:
- Topical Antifungal Agents: These are often effective for WSO since the infection is superficial and more accessible. Common treatments include ciclopirox, amorolfine, or efinaconazole.
- Oral Antifungal Medications: In cases where topical treatments are ineffective, or if the infection is extensive, oral antifungals like terbinafine or itraconazole may be prescribed.
Regular nail debridement and good nail hygiene are also important in managing WSO. Early diagnosis and treatment are crucial to prevent the infection from spreading or causing more severe nail damage.
For more detailed information, you can refer to resources such as the Mayo Clinic and American Academy of Dermatology.
What is proximal subungual onychomycosis?
Proximal subungual onychomycosis (PSO) is a less common form of fungal nail infection that primarily affects the proximal nail fold area, which is the region near the cuticle. Unlike other types of onychomycosis that usually start at the distal edge of the nail, PSO begins closer to the nail matrix, where the nail grows from. This type of onychomycosis is often associated with immunocompromised individuals, such as those with HIV/AIDS, and can be an indicator of systemic immunosuppression.
Key Characteristics and Symptoms
- White or Yellow Discoloration Near the Cuticle:
- PSO typically presents with a white or yellowish discoloration starting near the cuticle. This discoloration progresses outward as the nail grows.
- Nail Thickening:
- The infected area may thicken, similar to other forms of onychomycosis. However, because the infection starts near the cuticle, the thickening can affect the entire nail plate as the infection spreads.
- Onycholysis:
- Onycholysis, or the separation of the nail from the nail bed, can occur in PSO. This separation usually begins near the proximal nail fold and can lead to further complications if untreated.
- Subungual Hyperkeratosis:
- This condition involves the buildup of keratin under the nail, causing further thickening and possibly lifting the nail plate.
- Pain and Discomfort:
- While not always present, PSO can sometimes cause pain or discomfort, especially if the infection becomes severe and leads to significant nail changes.
Causes
Proximal subungual onychomycosis is often caused by dermatophytes, with Trichophyton rubrum being the most common causative agent. However, unlike other forms of onychomycosis, PSO can also be caused by non-dermatophyte molds and yeasts, especially in patients with compromised immune systems. The fungi invade the nail through the proximal nail fold, an area that is normally well-protected.
Risk Factors
- Immunocompromised States:
- PSO is strongly associated with immunocompromised conditions. Individuals with HIV/AIDS, those undergoing chemotherapy, or those on immunosuppressive drugs are at higher risk.
- Systemic Diseases:
- Conditions like diabetes, which can affect immune function, also increase the risk of developing PSO.
- Nail Trauma:
- Any damage to the nail matrix or proximal nail fold can provide an entry point for fungi, leading to PSO.
- Poor Nail Hygiene:
- Inadequate nail care can also contribute to the development of PSO, especially in individuals with other predisposing factors.
Diagnosis
Diagnosing PSO involves a combination of clinical examination and laboratory tests:
- Clinical Examination:
- A healthcare provider examines the nails for signs of infection, including discoloration, thickening, and onycholysis, with a focus on the proximal nail fold.
- Laboratory Tests:
- KOH Preparation: A sample of the affected nail area is treated with potassium hydroxide (KOH) to dissolve keratin, making it easier to visualize fungal elements under a microscope.
- Fungal Culture: This involves culturing a nail sample to identify the specific fungus causing the infection. This test is important for determining the appropriate treatment, especially if non-dermatophyte molds or yeasts are suspected.
- PCR Testing: Polymerase chain reaction (PCR) testing can identify fungal DNA, providing a rapid and accurate diagnosis.
Treatment
Treating PSO can be challenging, especially in immunocompromised patients. The treatment options include:
- Topical Antifungal Agents:
- These are often less effective for PSO due to the infection’s location near the nail matrix. However, they may be used in conjunction with other treatments.
- Oral Antifungal Medications:
- Oral antifungals like terbinafine, itraconazole, or fluconazole are typically required to treat PSO effectively. The treatment duration can be long, often several months, to ensure the infection is fully eradicated.
- Nail Removal:
- In severe cases, surgical removal of the affected nail may be necessary to allow for direct antifungal treatment of the nail bed.
- Adjunctive Therapies:
- Laser therapy and other adjunctive treatments may be considered, especially in cases where traditional treatments are not fully effective.
- Addressing Underlying Conditions:
- Managing underlying conditions, such as improving immune function or controlling diabetes, is crucial in preventing recurrence and promoting recovery.
For further reading, you can consult detailed sources such as the Mayo Clinic and American Academy of Dermatology. These resources provide comprehensive information on the diagnosis, treatment, and prevention of various forms of onychomycosis, including PSO.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!