Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!
Can onychomycosis affect both fingernails and toenails?
Yes, onychomycosis can affect both fingernails and toenails. However, it is more commonly seen in toenails due to several factors:
1. Environmental Factors
- Moisture and Warmth: Toenails are often exposed to environments that are more conducive to fungal growth, such as moist and warm conditions inside shoes. This creates an ideal environment for fungi to thrive and infect the nails.
- Reduced Airflow: Toenails receive less airflow compared to fingernails, which can increase moisture levels and encourage fungal growth.
2. Nail Trauma
- Toenail Trauma: Toenails are more prone to trauma from tight shoes or physical activities, which can damage the nail bed and provide an entry point for fungi. This trauma can be a significant risk factor for the development of onychomycosis.
3. Immunological Factors
- Weaker Immune Response in Toenails: The immune response in the toenail area might be less robust than in the fingernails, making toenails more susceptible to infection.
4. Hygiene Practices
- Less Frequent Cleaning: People may pay less attention to the hygiene of their feet and toenails compared to their hands and fingernails, potentially increasing the risk of fungal infections in toenails.
Fingernail Onychomycosis: While less common than toenail onychomycosis, fingernail infections do occur and are often associated with yeast infections, particularly Candida species. These infections are more likely in individuals who frequently immerse their hands in water, use artificial nails, or have underlying health conditions that compromise their immune system.
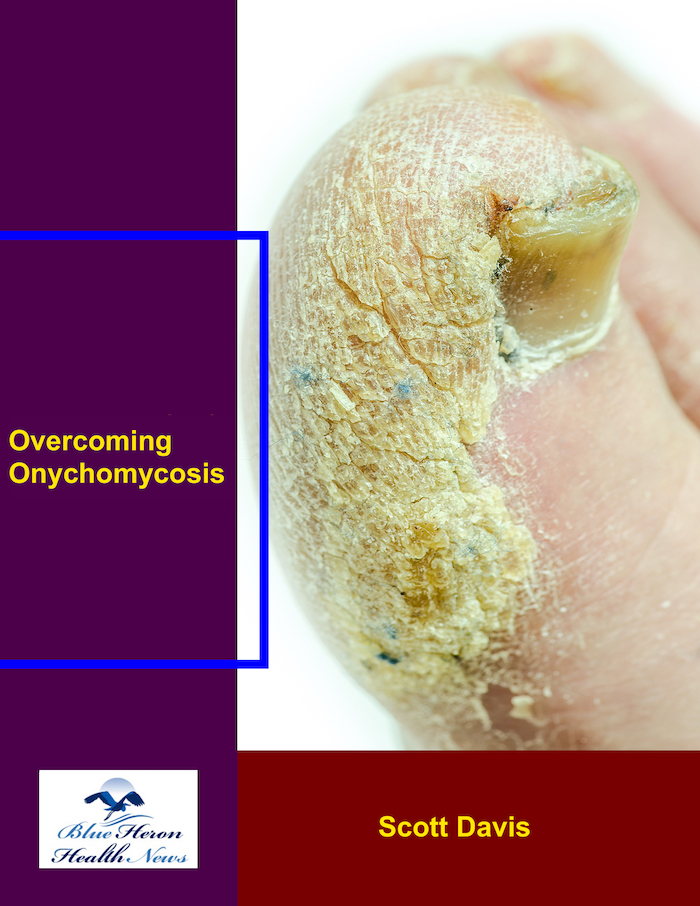
Clinical Presentation: The symptoms of onychomycosis in both fingernails and toenails include discoloration, thickening, brittleness, and separation of the nail from the nail bed (onycholysis). The clinical management and treatment approach can vary depending on whether the infection is in the fingernails or toenails.
For more information on onychomycosis, including treatment options and preventive measures, you can refer to the Mayo Clinic and the American Academy of Dermatology.
What are the different types of onychomycosis?
Onychomycosis, a fungal infection of the nails, can present in several distinct types, each with unique characteristics and causes. The main types of onychomycosis include:
1. Distal Subungual Onychomycosis (DSO)
- Description: This is the most common form of onychomycosis. It starts at the end of the nail (distal edge) and progresses under the nail towards the cuticle. It often affects the toenails but can also occur in fingernails.
- Symptoms: Nail thickening, discoloration (yellow or white), and onycholysis (separation of the nail from the nail bed).
- Causes: Typically caused by dermatophytes, particularly Trichophyton rubrum.
2. White Superficial Onychomycosis (WSO)
- Description: This type involves the surface of the nail plate, often affecting the toenails.
- Symptoms: White, chalky patches or spots on the nail surface that may be easily scraped off.
- Causes: Commonly caused by non-dermatophyte molds and sometimes dermatophytes.
3. Proximal Subungual Onychomycosis (PSO)
- Description: This less common form starts near the cuticle area and spreads outward. It is often seen in individuals with compromised immune systems.
- Symptoms: White spots near the cuticle, nail thickening, and possible onycholysis.
- Causes: Can be caused by dermatophytes and, less commonly, by non-dermatophyte molds.
4. Candidal Onychomycosis
- Description: Caused by yeast, particularly Candida species. It often affects fingernails and can be associated with chronic mucocutaneous candidiasis.
- Symptoms: Whitish or yellowish discoloration, nail thickening, and onycholysis. The surrounding skin may also be affected, leading to paronychia (inflammation of the nail fold).
- Causes: Typically associated with Candida albicans and other Candida species.
5. Total Dystrophic Onychomycosis
- Description: This is the most severe form of onychomycosis and represents the end stage of any of the aforementioned types.
- Symptoms: Complete destruction of the nail, severe thickening, and discoloration. The nail may crumble and detach entirely.
- Causes: It can result from untreated or severe cases of DSO, PSO, or WSO.
These types can overlap, and a single nail can sometimes be affected by more than one form of onychomycosis. Accurate diagnosis often requires clinical examination and laboratory tests, such as culture, KOH preparation, or PCR, to determine the specific type and causative agent. This helps guide appropriate treatment, which can vary based on the type of fungus involved.
For further reading and more detailed information, you can refer to Mayo Clinic and the American Academy of Dermatology.
What is distal subungual onychomycosis?
Distal subungual onychomycosis (DSO) is the most common type of fungal nail infection. It primarily affects the toenails but can also occur in fingernails. DSO involves the distal edge of the nail, starting at the tip and gradually spreading towards the cuticle. The infection affects both the nail plate and the underlying nail bed.
Key Characteristics and Symptoms
- Nail Discoloration:
- One of the hallmark symptoms of DSO is discoloration of the nail. The nail may appear yellow, brown, or white. This discoloration typically begins at the distal (far) end of the nail and progresses towards the cuticle.
- Nail Thickening:
- The infected nail often becomes thickened, making it difficult to trim and maintain. This thickening results from the accumulation of fungal material and debris under the nail.
- Onycholysis:
- Onycholysis, or the separation of the nail from the nail bed, is a common feature of DSO. This separation can create a gap under the nail where additional debris and fungal material accumulate, exacerbating the infection.
- Brittleness and Crumbling:
- Affected nails may become brittle and crumble easily. This brittleness can lead to jagged edges and an irregular nail surface.
- Subungual Hyperkeratosis:
- This condition involves the thickening of the skin under the nail, further lifting the nail from the nail bed and contributing to the nail’s distorted appearance.
Causes
DSO is primarily caused by dermatophytes, which are fungi that thrive on keratin, the protein that makes up nails and skin. The most common dermatophyte responsible for DSO is Trichophyton rubrum, but other species like Trichophyton mentagrophytes can also cause the condition.
Risk Factors
Several factors increase the risk of developing DSO, including:
- Age: Older adults are more susceptible due to slower nail growth and decreased blood circulation.
- Environmental Factors: Frequent exposure to warm, moist environments, such as communal showers, swimming pools, or locker rooms.
- Nail Trauma: Injuries to the nail can provide an entry point for fungi.
- Underlying Health Conditions: Conditions like diabetes or immunosuppression can increase the risk of fungal infections.
Diagnosis and Treatment
Diagnosis typically involves a physical examination and laboratory tests, such as a KOH (potassium hydroxide) preparation, fungal culture, or PCR (polymerase chain reaction) testing. These tests help confirm the presence of fungal elements and identify the specific type of fungus causing the infection.
Treatment options for DSO include topical antifungal medications, oral antifungal drugs, and in some cases, laser therapy or surgical removal of the affected nail. The choice of treatment depends on the severity of the infection, the specific fungus involved, and patient-specific factors.
For more detailed information, consult resources like the Mayo Clinic and American Academy of Dermatology.
Overcoming Onychomycosis™ By Scott Davis If you want a natural and proven solution for onychomycosis, you should not look beyond Overcoming Onychomycosis. It is easy to follow and safe as well. You will not have to take drugs and chemicals. Yes, you will have to choose healthy foods to treat your nail fungus. You can notice the difference within a few days. Gradually, your nails will look and feel different. Also, you will not experience the same condition again!